Session Information
Date: Saturday, November 16, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The journey to axial spondyloarthritis (axSpA) diagnosis is often prolonged and challenging, resulting in poor clinical, psychological, social, and economic outcomes.1 Understanding the factors contributing to delays is crucial to improve diagnostic pathways and outcomes. Here, we evaluate time to axSpA diagnosis and the patient journey from earliest back pain diagnosis to axSpA diagnosis in the US.
Methods: This observational, retrospective, US MarketScan study used insurance claims data from the CCAE/MDCR (Jan 2008–Mar 2023) and Medicaid (Jan 2008–Dec 2022) databases. Adult patients with ≥5 years of medical and pharmacy benefit utilized, and back pain onset prior to a new axSpA diagnosis were included.
We report time to diagnosis (earliest back pain diagnosis to first axSpA diagnosis), and duration of primary (earliest back pain diagnosis to the first rheumatology visit) and secondary delay (first rheumatology visit to first axSpA diagnosis).
Diagnostic journeys from earliest back pain diagnosis to axSpA diagnosis were described by number of back pain episodes recorded on separate days, number and type of all-cause and back pain-related specialist visits, and all-cause diagnostic tests (HLA-B typing, ESR, CRP) and imaging procedures (X-ray, CT scan, MRI of the spine or pelvis).
Results: This study included 97,469 patients, with a mean (SD) age of 48.8 (14.9) years at earliest back pain diagnosis, and 53.2 (14.9) years at axSpA diagnosis; 63.7% were female.
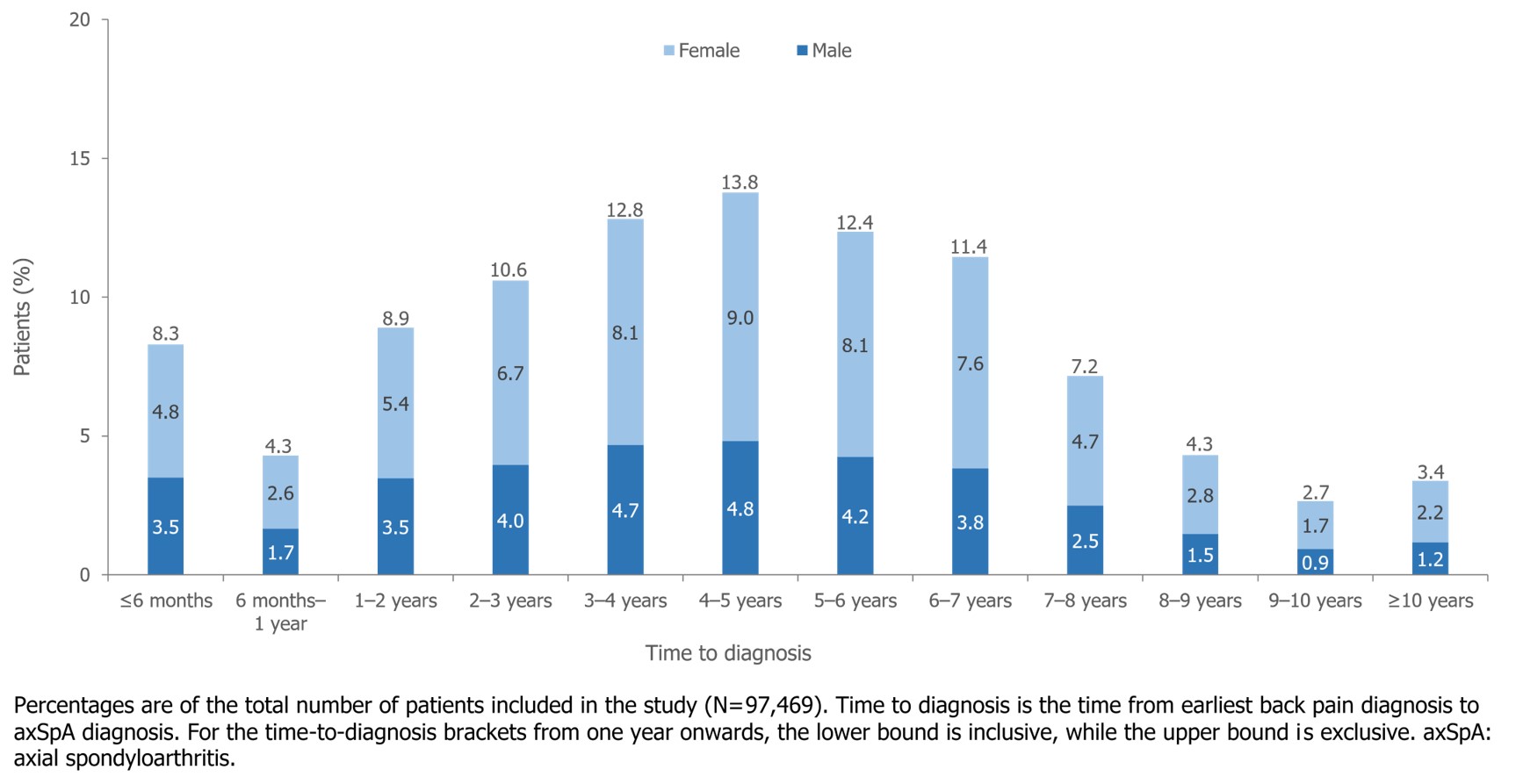
Of the cohort, 41.3% had a total time to diagnosis ≥5 years (Figure 1); median (Q1, Q3) time to diagnosis was 4.35 (2.35, 6.34) years. Among the 9,824 (10.1%) patients who saw a rheumatologist before axSpA diagnosis, median primary delay was 2.62 (1.07, 4.60) years, and secondary delay was 1.69 (0.24, 3.72) years.
Between earliest back pain and axSpA diagnosis, median (Q1, Q3) number of back pain episodes was 13 (5, 28) and 58.7% of patients experienced ≥10 back pain episodes.
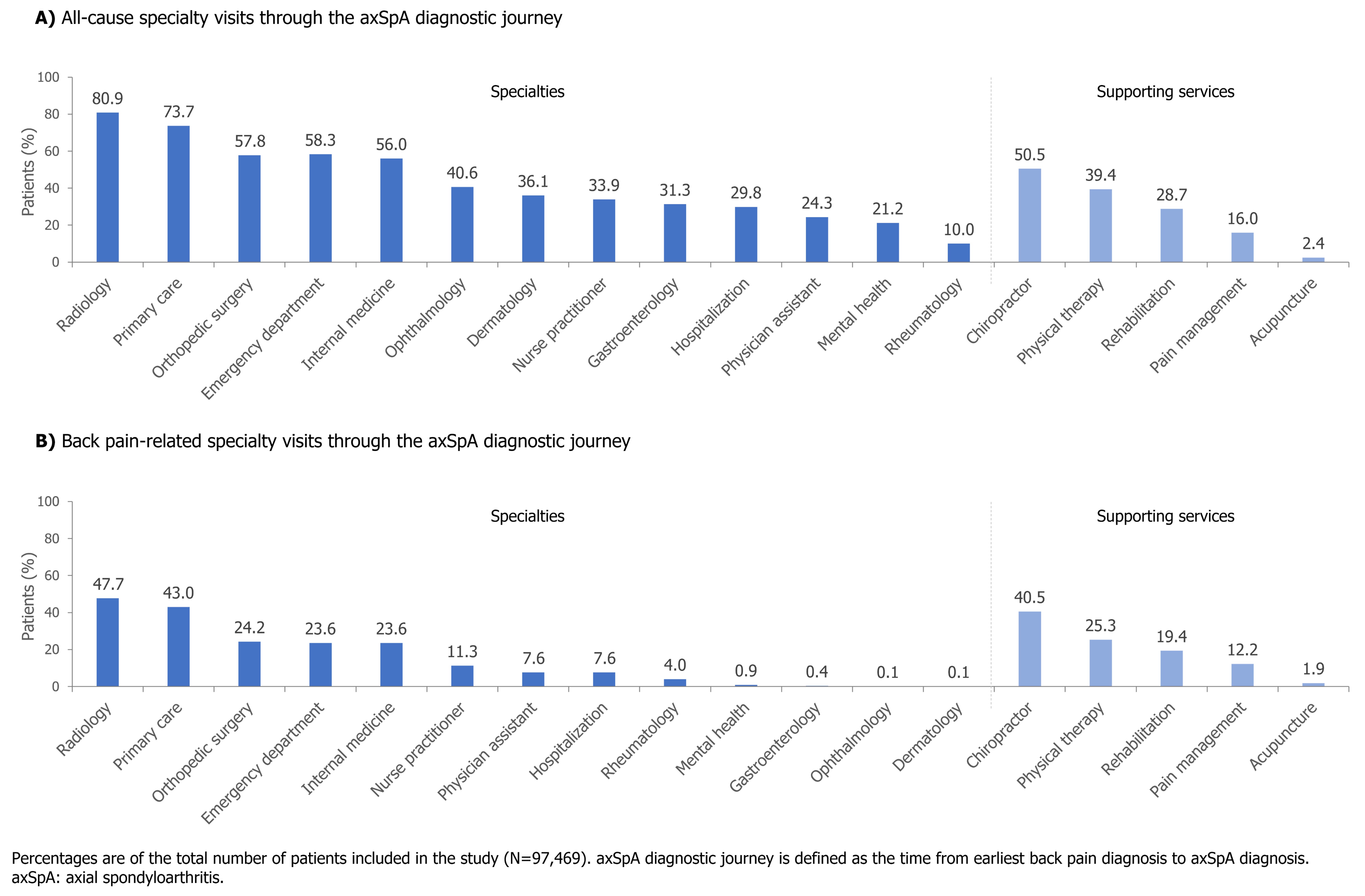
Patients saw a range of specialists in their diagnostic journey, including rheumatology, orthopedic surgery, dermatology, and gastroenterology (Figure 2A). Of back pain-related specialist visits (Figure 2B), the rate (95% CI) of visits per year from the earliest back pain diagnosis to axSpA diagnosis was 3.73 (3.73, 3.74); this included 0.40 (0.40, 0.40) back pain-related primary care visits per year.
Patients had a range of diagnostic tests and imaging procedures, with a mean (SD) of 0.02 (0.15) HLA-B typing, 0.76 (2.24) ESR, and 0.54 (2.01) CRP tests, and 2.32 (2.68) X-rays, 0.27 (0.79) CTs, and 0.99 (1.44) MRIs per patient.
Conclusion: Early axSpA diagnosis is crucial for timely access to care and treatment. This study shows that diagnostic delay is a challenge for patients with axSpA in the US, despite numerous back pain consultations, specialist visits, and diagnostic tests. Additionally, secondary delay after seeing a rheumatologist was also high. This study highlights the need for medical education on inflammatory back pain and axSpA, and the development of patient pathways to reduce the disease burden on patients and the healthcare system.
References: 1. Yi E. Rheumatol Ther 2020;7:65–87.
To cite this abstract in AMA style:
Dubreuil M, Magrey M, Haeffs K, Ivanov E, Gandrup Horan J. Patient Diagnostic Journey and Time to Diagnosis in Axial Spondyloarthritis: A Retrospective Cohort Study Using US Claims Data [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-diagnostic-journey-and-time-to-diagnosis-in-axial-spondyloarthritis-a-retrospective-cohort-study-using-us-claims-data/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-diagnostic-journey-and-time-to-diagnosis-in-axial-spondyloarthritis-a-retrospective-cohort-study-using-us-claims-data/