Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Advances in treatment of juvenile-onset systemic lupus erythematosus have ensured increased survival such that long-term quality of life and disease management must be considered. Interventions to improve jSLE transition outcomes require an understanding of the challenges faced by patients and their health care teams during this time.
In this qualitative study, we had a unique opportunity to interview uninsured or publicly insured young adults with jSLE who recently transitioned to adult rheumatology care, along with health care professionals caring for pediatric and adult jSLE patients. Interviews identified influential factors affecting pediatric-to-adult rheumatology transition success. A subset of influential factors are described herein, organized under the conceptual frameworks of patient activation and health literacy (HL). Recommendations to improve transition success were also elicited from each cohort.
Methods: Semi-structured in-depth interviews with patients and health care professionals were conducted from November 2019 – May 2020, until thematic saturation. Thirteen post-transfer adult participants diagnosed with jSLE (in concordance with 2019 EULAR/ACR classification) were recruited from a public safety-net hospital system or from private practice. Thirteen health care team members were recruited from two pediatric and four adult rheumatology clinical sites in the same metropolitan area. Interviews were recorded, transcribed, coded, and analyzed using thematic analysis.
Results: Our interviews suggest that patient activation is driven by internalization of the implications of jSLE diagnosis, capacity and willingness to engage in self-education, autonomy, introspection, and trustworthy doctor-patient relationships (Table 1). Patients and health professionals acknowledged numerous HL components as determinants of transition success, including: language fluency and baseline education, extent of SLE-specific knowledge, self-efficacy (ability to make appointments, fill prescriptions, and obtain and utilize insurance), and accurate knowledge of personal medical history (Table 2). When asked how to improve the transition process, patients valued access to their secure online electronic medical record and recommended multimodal SLE-specific educational materials and increased access to social work services (Table 3). Health care professionals stressed the importance of early preparation for transition, utilization of mobile medical applications, and endorsed interventions such as lupus camp and increased partnership with psychologists and social workers (Table 3).
Conclusion: Patient activation and HL are acknowledged by patients and health care teams as substantially influencing pediatric-to-adult transition success among an uninsured/publicly insured urban jSLE cohort. Further research is needed to evaluate whether improved patient activation and HL positively influence jSLE transition outcomes.
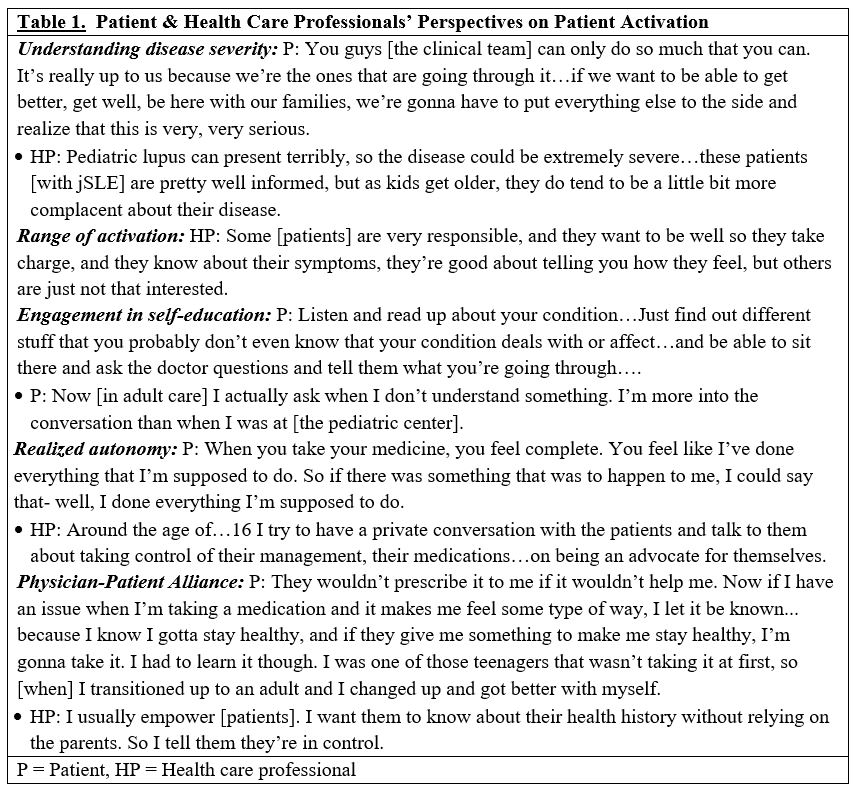 Patient & Health Care Professionals’ Perspectives on Patient Activation
Patient & Health Care Professionals’ Perspectives on Patient Activation
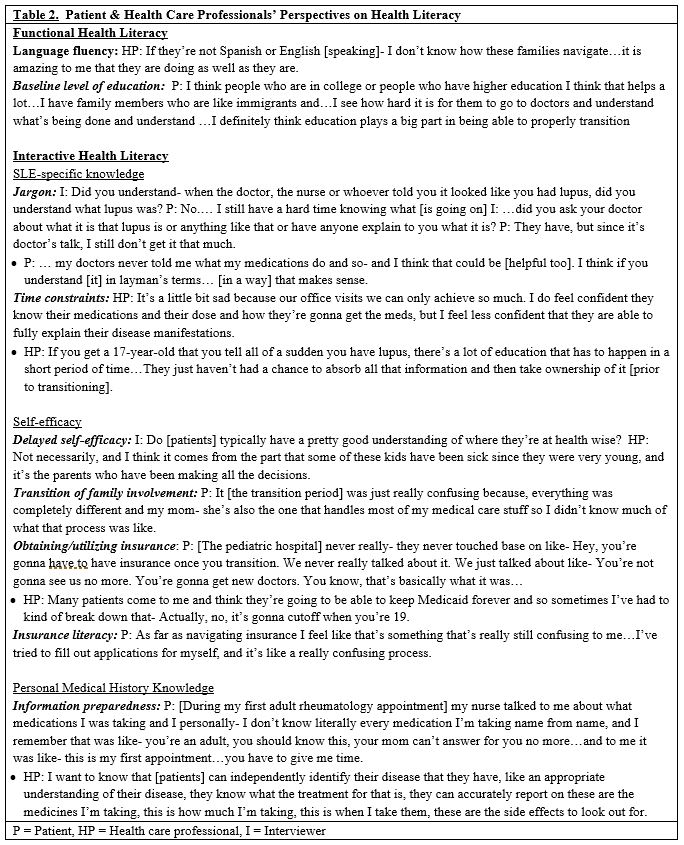 Patient & Health Care Professionals’ Perspectives on Health Literacy
Patient & Health Care Professionals’ Perspectives on Health Literacy
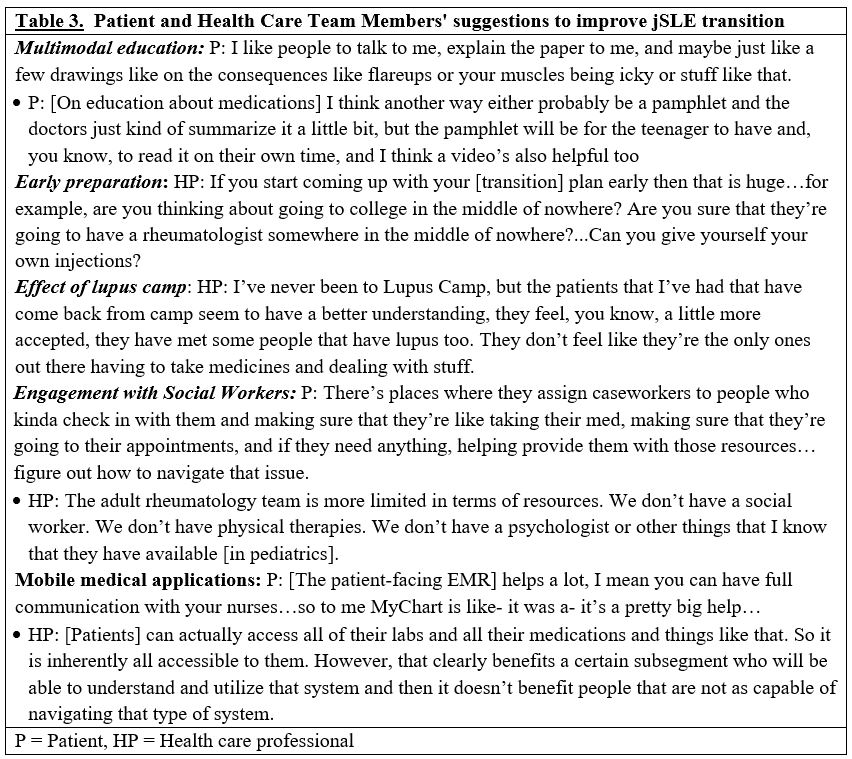 Patient & Health Care Team Members’ Suggestions to Improve jSLE Transition
Patient & Health Care Team Members’ Suggestions to Improve jSLE Transition
To cite this abstract in AMA style:
Ciosek A, Makris U, Kramer J, Wright T, Bitencourt N. Patient Activation and Health Literacy in the Pediatric to Adult Transition in Juvenile Systemic Lupus Erythematosus: Patient and Health Care Team Perspectives [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/patient-activation-and-health-literacy-in-the-pediatric-to-adult-transition-in-juvenile-systemic-lupus-erythematosus-patient-and-health-care-team-perspectives/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-activation-and-health-literacy-in-the-pediatric-to-adult-transition-in-juvenile-systemic-lupus-erythematosus-patient-and-health-care-team-perspectives/
