Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pain is the most common symptom among patients with inflammatory arthritis (IA) and residual pain is common in patients IA despite appropriate treatment. Opiate pain medications have been used in the past to assist in managing patients’ pain but have increasingly been recognized as potentially harmful medications. The objectives of this study were to a) examine pain perception among patients with RA, PsA, and AS and b) to examine the prevalence and incidence of opiate pain mediation use between 2001-2018 among patients with IA.
Methods: Using data from Forward/National Data Bank for Rheumatic Diseases between 2001-2018, a cross-sectional study was performed using the most recent visit for patients with AS, PsA, or RA with a rheumatologist confirmed diagnosis. Additionally, a retrospective cohort study was performed in the same cohort to examine time trends in the prevalence and incidence of opiate use. Participants in Forward complete questionnaires every 6 months that include patient reported outcome (PRO) measures such as PROMIS29, a wide spread pain index, and a survey of medications used, including pain medications. Incident opiate use was defined as having no prior report of opiate use in previous questionnaires with at least one completed questionnaire prior to the first report of opiate use. Mean and standard deviations for PRO scores were reported for each group and a Kruskal Wallis test or chi2 test was used to determine whether significant differences existed (for continuous and categorical outcomes respectively).
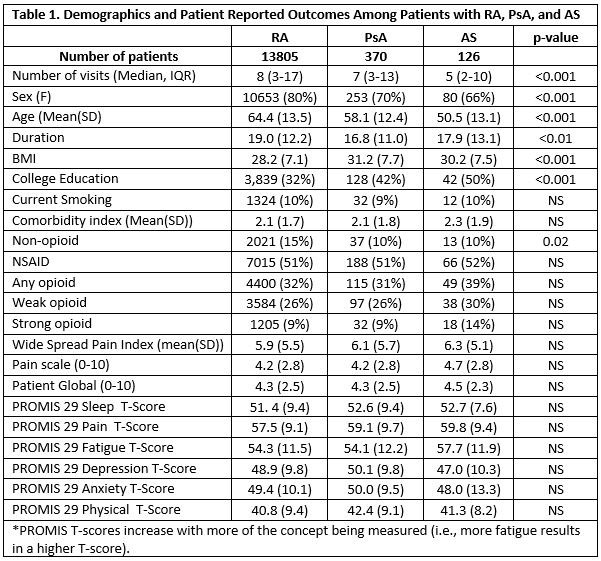
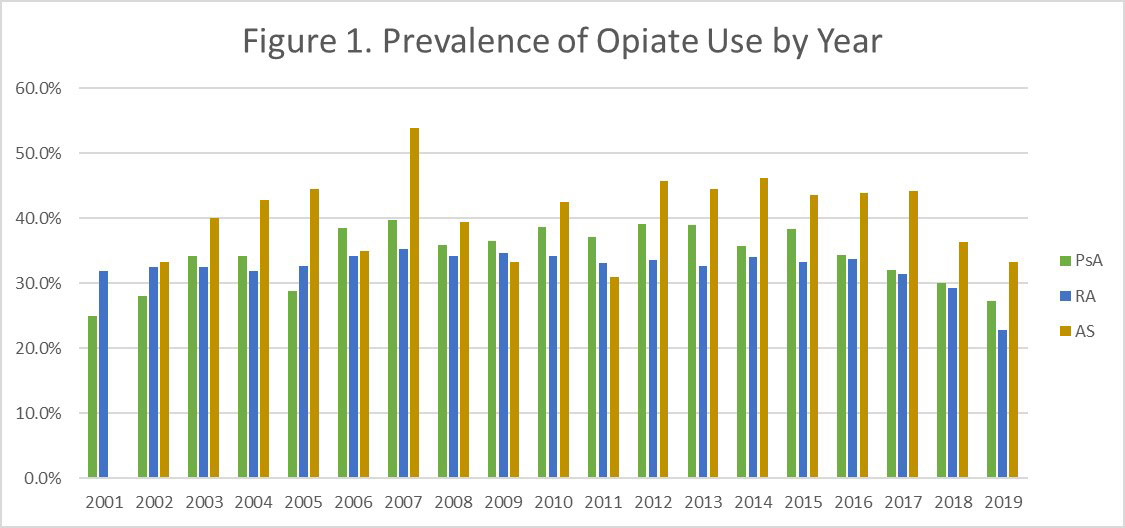
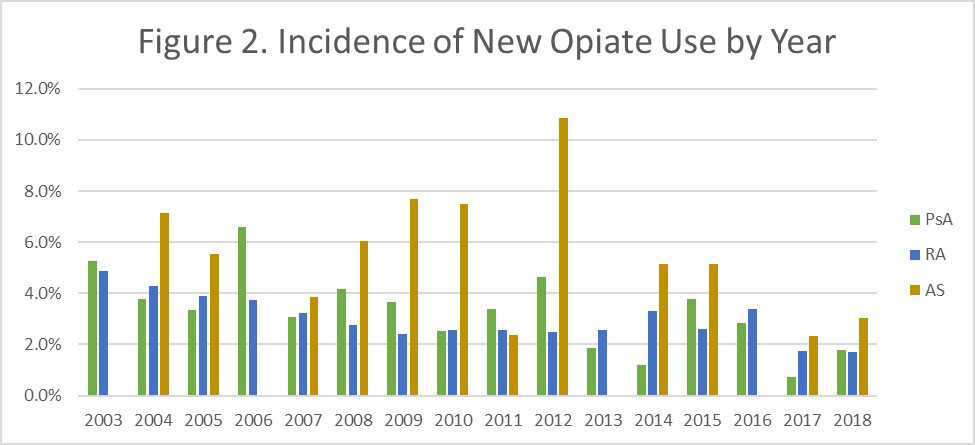
Results: Among those enrolled in Forward, 13,805, 370, and 126 patients with RA, PsA, and AS respectively met eligibility criteria for this study. Patients with RA generally had more follow up time and were older (mean age 64 vs 58 and 50 respectively) and more likely to be female (80% vs 70% and 66% respectively). In general, pain scores (pain numeric rating scale, PROMIS29 pain score, wide spread pain index, Table 1) were statistically similar across the three diseases but numerically higher in AS. Patients with PsA had higher depression scores while patients with AS had higher fatigue scores. While more patients with RA were using non-opioid pain medications at their most recent survey time point, more patients with AS reported taking an opioid pain medication. In most years, patients with AS were more likely to be taking opioid pain medications and this was statistically significant overall (p=0.01). AS patients also had a higher incidence of new opioid use. In general, for all three diseases, new opiate use has been declining over the past 3 years.
Conclusion: In this study among patients with IA, statistically similar levels of pain, fatigue, sleep, depression and anxiety were reported though AS patients had numerically higher pain scores. Patients with AS received more opioid medications. However, in general, opioid use has been declining in the last three years.
To cite this abstract in AMA style:
Ogdie A, Pedro S, Michaud K. Pain Perception and Opiate Use Among Patients with Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/pain-perception-and-opiate-use-among-patients-with-inflammatory-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pain-perception-and-opiate-use-among-patients-with-inflammatory-arthritis/