Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with Rheumatoid arthritis (RA) have a higher burden of cardiovascular diseases (CVDs) than the general population, with most deaths resulting from myocardial infarctions. There are conflicting results of previous studies about in-hospital outcomes of STEMI in patients with RA compared to patients without RA. This study aimed to compare in-hospital outcomes of the first episode of STEMI between patients with and without RA.
Methods: The NIS database represents a 20% stratified sample, or approximately 35 million U.S. hospital discharges annually. We conducted a retrospective study of hospitalizations with a primary diagnosis of STEMI and excluded patients with prior coronary artery disease (percutaneous coronary intervention [PCI], coronary artery bypass graft, or myocardial infarction) to capture only the first STEMI from 2016 to 2019. Our study population was then divided into two comparative cohorts, with RA, and without RA. We compared the two groups’ baseline demographics, comorbidities, and in-hospital outcomes. Continuous variables were expressed as mean, while categorical variables were represented in the percentage of the total population. Differences between groups were tested for continuous and categorical variables using t-test and Chi-square tests. Subsequently, we performed a multivariate logistic regression analysis for the same outcomes, adjusting for baseline factors significantly different (p< 0.1) in baseline characteristics by univariate analysis. Results of regression analyses were expressed as odds ratios (OR) with respective confidence intervals (CI) and p-values.
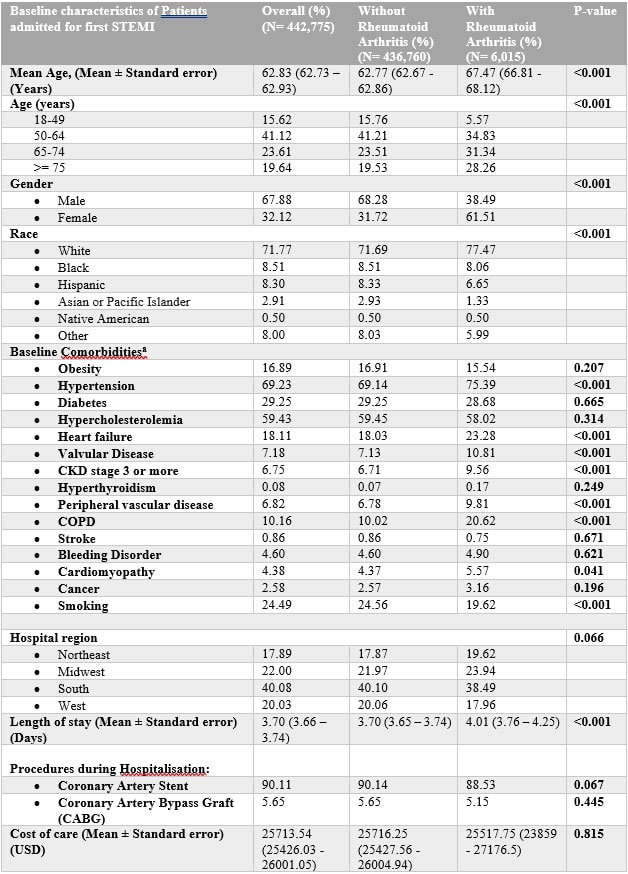
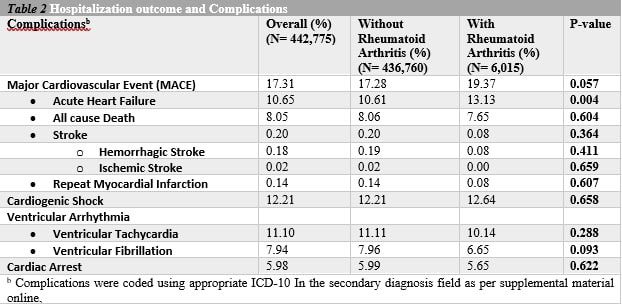
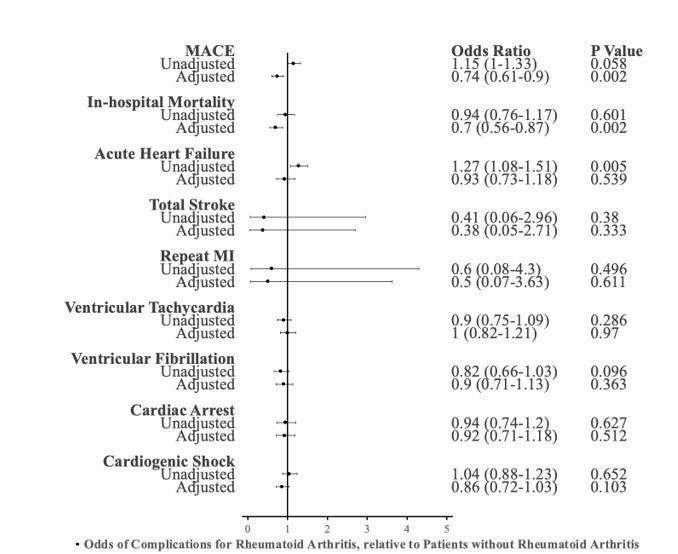
Results: Our analysis revealed that patients with RA were statistically more likely to be older, white, and female (Table 1). Interestingly, after adjusting for potential confounders with multivariable regression analysis, we found lower inpatient mortality in the first STEMI with RA cohort (adjusted OR: 0.74, 95% CI of 0.61-0.9, P value< 0.002) compared to the patients without RA (Table 2). However, there was no statistically significant difference between the two groups regarding complications, including repeat MI, acute heart failure, ventricular tachycardia, ventricular fibrillation, cardiac arrest, cardiogenic shock, and stroke during that hospitalization (Figure 1). Furthermore, there was no significant difference between groups in receiving invasive procedures, including coronary artery stenting (88.53 % vs. 90.14%, p-value 0.07) and coronary artery bypass (5.15% in RA vs. 5.65 % Non- RA patients, p-value: 0.45) (Table 1). Additionally, the annual mortality rate in patients with RA did not significantly change between 2016 and 2019 (average annual percentage change, –0.07%; P = 0.06). Also, we found no significant difference in the total length of stay between the two groups.
Conclusion: This nationwide study suggests that patients with RA with first STEMI have lower inpatient mortality than those without RA. However, further patient-level studies are needed to understand better the impact of newer biologics and the effect of risk factor modification on this patient subset.
a: Comorbidities were coded using appropriate ICD_10 In the secondary diagnosis field as per supplemental material online
* Adjusted for age, race, female, heart failure, hypertension, COPD, peripheral vascular disease, valvular heart disease, cardiomyopathy, smoking
To cite this abstract in AMA style:
Suwal A, Shrestha B, Oke I, Donato A. Outcomes of the First Episode of STEMI in Rheumatoid Arthritis from the National Inpatient Sample Database 2016-2019 [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-the-first-episode-of-stemi-in-rheumatoid-arthritis-from-the-national-inpatient-sample-database-2016-2019/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-the-first-episode-of-stemi-in-rheumatoid-arthritis-from-the-national-inpatient-sample-database-2016-2019/