Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Respiratory Syncytial Virus (RSV) can cause a severe respiratory illness, especially in older adults and those with significant comorbidities. In June 2023 the US CDC recommended that all adults 60 years and older receive the RSV vaccination. However, there is little evidence regarding RSV outcomes among people with systemic autoimmune rheumatic diseases (SARDs), particularly those using disease-modifying antirheumatic drugs (DMARDs). Our objective was to describe the clinical outcomes of RSV infections in patients with SARDs and identify factors associated with hospitalization during an RSV infection.
Methods: We performed a retrospective study in a large multicenter healthcare system. Among all patients with a positive test for RSV between 6/2015 and 11/2023, we identified those with a SARD at the time of infection, using a previously validated algorithm and confirmed by chart review. The electronic health record was manually reviewed to evaluate exposures of interest and to determine the outcome as well as cause of death. The primary outcome was requiring hospitalization during RSV infection. We evaluated baseline factors associated with hospitalization for RSV, including demographics, SARD treatment and characteristics, comorbidities, and concurrent infection. We used logistic regression to assess the association of these baseline factors with the odds of hospitalization with RSV.
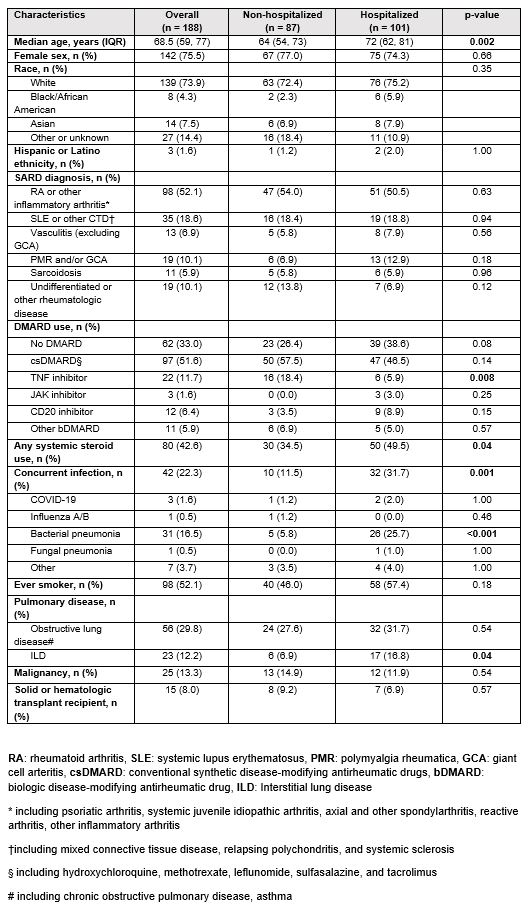
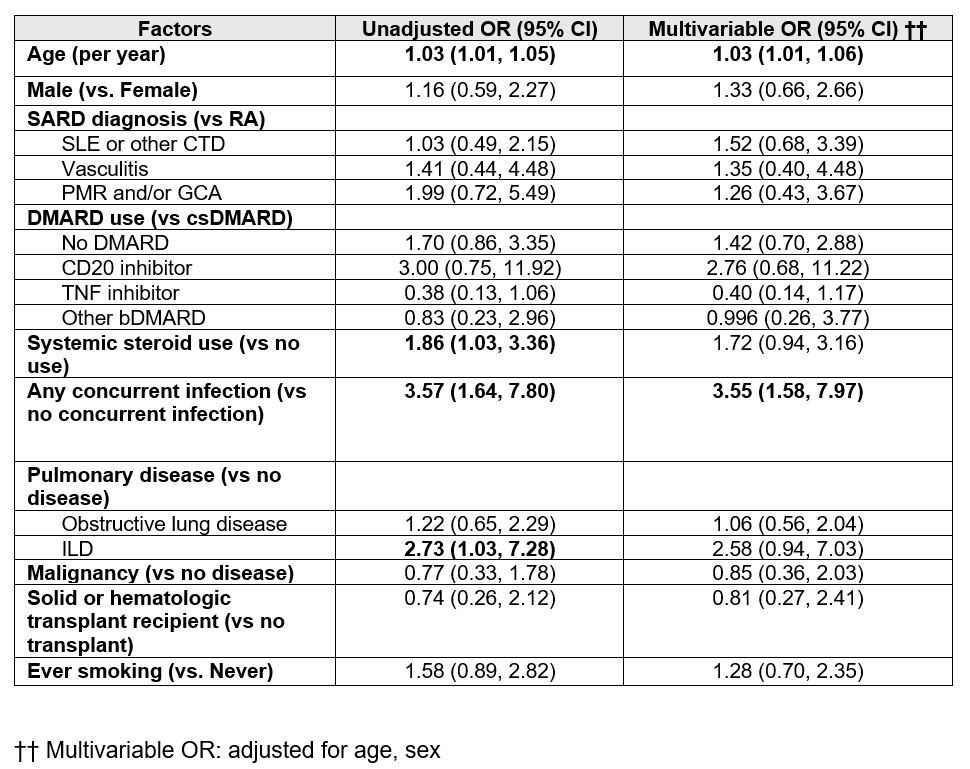
Results: We included 188 individuals with SARDs and confirmed RSV infection (mean age 68.5 years, 76% female). The most common SARD type was inflammatory arthritis (52%). The most common rheumatologic treatments were conventional synthetic DMARDs and systemic glucocorticoids in 97 (52%) and 80 (43%) patients, respectively. 42 patients (22%) had a concurrent viral, bacterial, or fungal infection. 101 patients (54%) were hospitalized during their RSV infection; 85% of hospitalizations were for RSV or infection-related complications (Table 1). Older age (aOR 1.03) and concurrent infection (aOR 3.55) were associated with hospitalization (Table 2). There were trends towards associations between CD20-inhibitor therapy and interstitial lung disease (ILD) with the odds of hospitalization. Of those using CD20 inhibitors (n=12), 9 (75%) were hospitalized. Of those with ILD (n=23), 17 (74%) were hospitalized. 12 patients (6%) died within 90 days of RSV infection; 8 deaths were attributed to RSV.
Conclusion: In this first investigation of RSV outcomes among patients with SARDs, older age, ILD, and CD20 inhibitors were identified as potential risk factors for RSV hospitalization. Our study underscores the interplay between host vulnerability factors in rheumatologic patients with outcomes of RSV infection. These findings provide support for ongoing efforts to expand approval for RSV vaccination for people under age 60 years with significant risk factors for severe RSV infection.
To cite this abstract in AMA style:
Enns J, Srivatsan S, Jiang B, Lin M, Kowalski E, Patel N, Wang X, Williams Z, Qian G, Hanberg J, Johnson C, Negron M, Bade K, Saavedra A, Mueller K, Vanni K, Sparks J, Wallace Z. Outcomes of Respiratory Syncytial Virus Infection in Patients with Systemic Autoimmune Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-respiratory-syncytial-virus-infection-in-patients-with-systemic-autoimmune-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-respiratory-syncytial-virus-infection-in-patients-with-systemic-autoimmune-rheumatic-diseases/