Session Information
Date: Monday, November 9, 2020
Title: Late-Breaking Posters
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The risk of poor outcomes from COVID-19 among rheumatic disease patients compared to the general population remains poorly understood. Filling this knowledge gap is a high priority for patients and providers. We previously observed a higher risk of mechanical ventilation in patients with rheumatic diseases compared to the general population in a small cohort study early in the pandemic.
Methods: We conducted a cohort study of COVID-19 patients (confirmed by polymerase chain reaction [PCR]) between January 30 and July 16, 2020, at a multicenter healthcare system including academic and community hospitals and longitudinal clinics. We compared each patient with systemic rheumatic disease to up to 5 matched (by age, sex, and date of COVID-19 PCR) comparators without rheumatic disease. In our primary analysis, we used multivariable Cox proportional hazard regression to estimate hazard ratios (HR) and 95% confidence intervals (CI) for COVID-19 outcomes, comparing patients with and without rheumatic disease and adjusting for potential confounders. Outcomes were evaluated through end of follow-up in the system or August 18, 2020. To further evaluate temporal trends in mechanical ventilation among rheumatic disease patients, we compared risk of this outcome in an early vs. recent cohort (PCR testing before vs. after the midpoint among rheumatic disease patients) using similar methods.
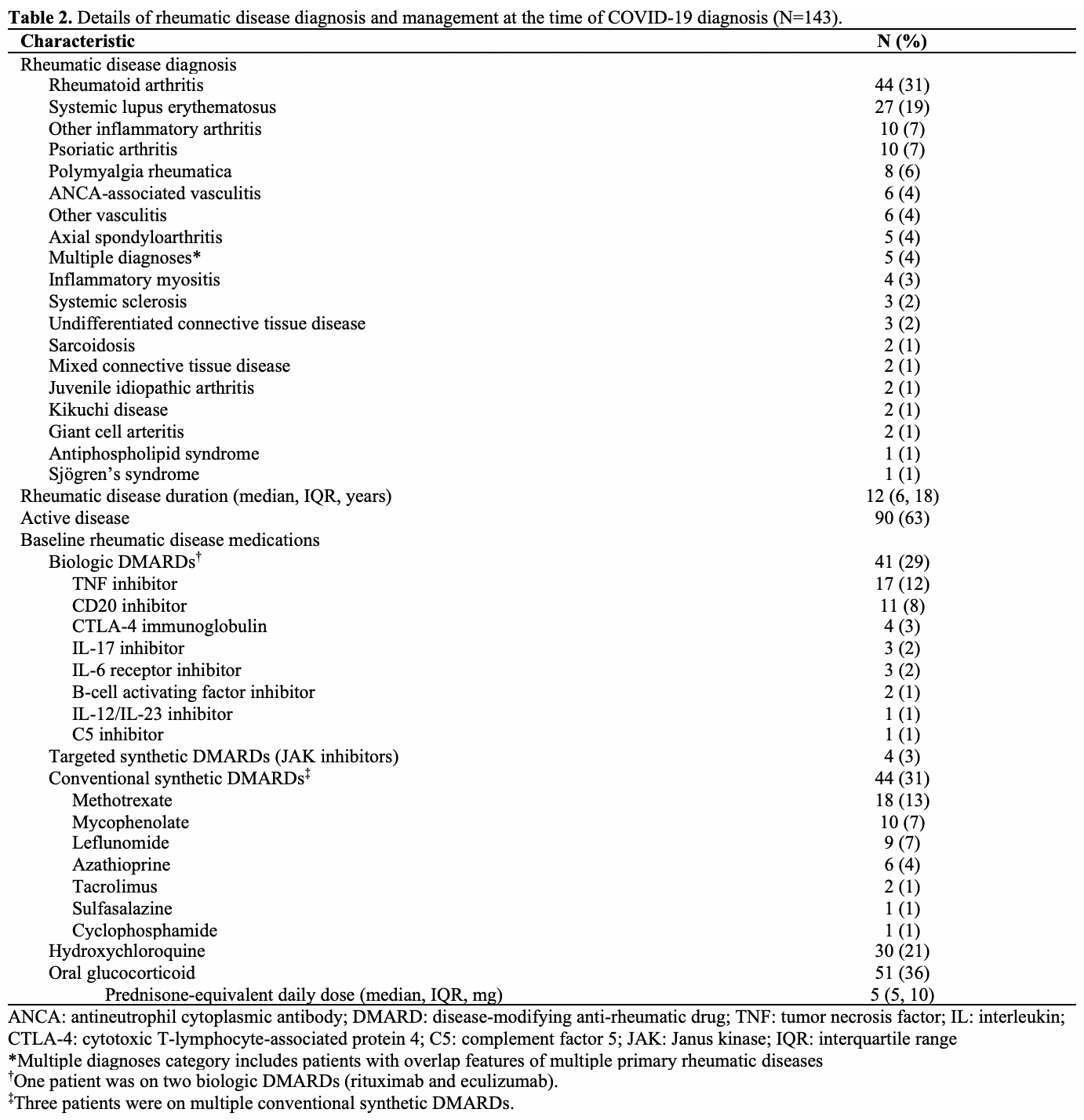
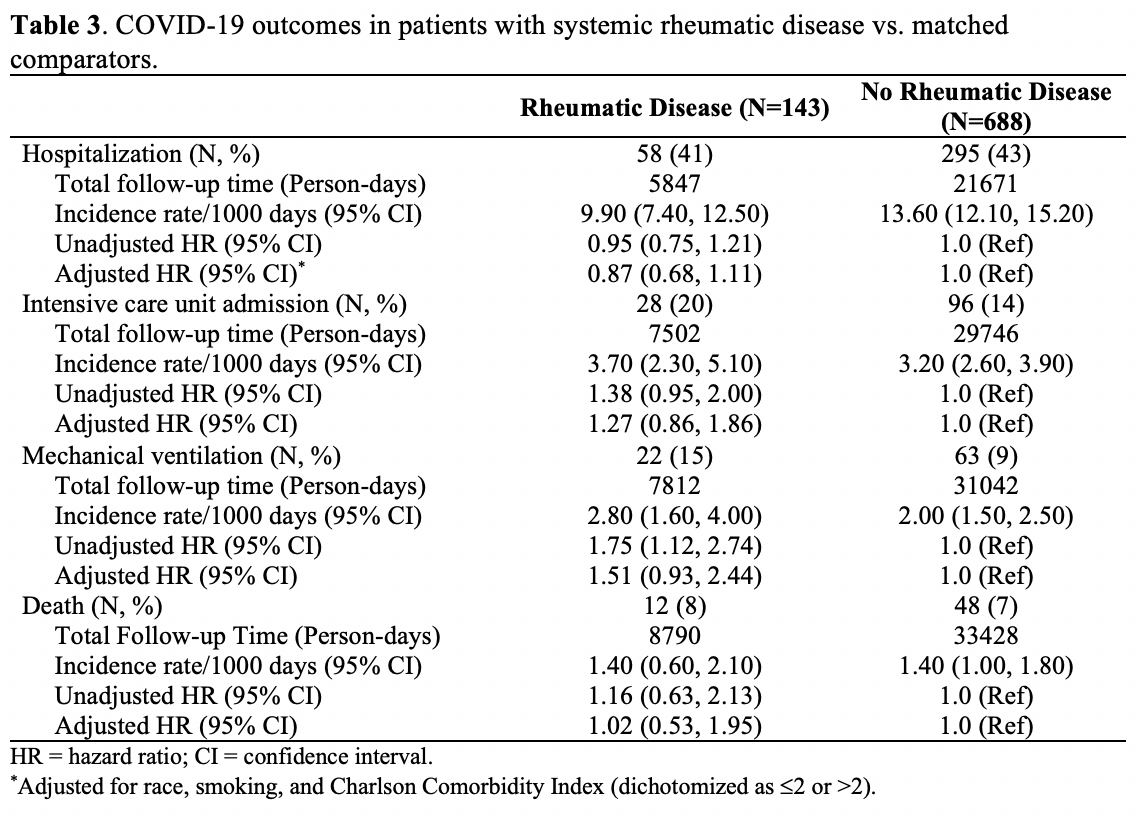
Results: We identified 143 rheumatic disease patients (mean age 60 years, 76% female) and 688 matched comparators (mean age 59 years, 76% female) out of 16,211 patients who had confirmed COVID-19 (Table 1). Median Charlson Comorbidity Index (CCI) scores and interquartile range (IQRs) were higher among patients with rheumatic disease (2 [IQR: 1, 4]) vs. comparators (0 [IQR: 0, 2]). The most common rheumatic diseases were rheumatoid arthritis (44, 31%) and systemic lupus erythematosus (27, 19%) (Table 2). Fifty-one (36%) rheumatic disease patients were on glucocorticoids, 30 (21%) were on hydroxychloroquine, 41 (29%) were on at least 1 biologic disease-modifying antirheumatic drug (DMARD), and 44 (31%) were on at least 1 conventional synthetic DMARD. Patients with rheumatic disease had higher unadjusted risk of mechanical ventilation than comparators (unadjusted HR 1.75, 95% CI: 1.12 to 2.74) (Table 3). After adjustment for race, smoking, and CCI, there were no significantly higher risks of hospitalization (HR 0.87, 95% CI: 0.68 to 1.11), intensive care unit admission (HR 1.27, 95% CI: 0.86 to 1.86), mechanical ventilation (HR 1.51, 95% CI: 0.93 to 2.44), or death (HR 1.02, 95% CI: 0.53 to 1.95) in rheumatic disease patients vs. comparators. We observed a trend toward improvement in the risk of mechanical ventilation in the recent vs. early rheumatic disease cohorts (10% vs. 19%, adjusted HR 0.44, 95% CI: 0.17 to 1.12).
Conclusion: Patients with rheumatic disease had similar risk of severe COVID-19 outcomes vs. comparators. There was a temporal trend toward improvement in risk of mechanical ventilation for rheumatic disease patients. These findings provide reassurance for rheumatic disease patients but close monitoring of rheumatic disease patients with other comorbidities is warranted.
To cite this abstract in AMA style:
Serling-Boyd N, D'Silva K, Hsu T, Fu X, Wallwork R, Jorge A, Zhang Y, Gravallese E, Choi H, Sparks J, Wallace Z. Outcomes of COVID-19 Infection in Patients with Rheumatic Diseases in a Multicenter Healthcare System: A Comparative Cohort Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-patients-with-rheumatic-diseases-in-a-multicenter-healthcare-system-a-comparative-cohort-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-patients-with-rheumatic-diseases-in-a-multicenter-healthcare-system-a-comparative-cohort-study/