Session Information
Date: Monday, November 13, 2023
Title: (1052–1081) Immunological Complications of Medical Therapy Poster
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Coronavirus disease 2019 (COVID-19) can have varying outcomes. Patients with chronic conditions or immunosuppression experience more severe illness. Both organ transplant recipients and patients with certain autoimmune rheumatic diseases (ARD) require immunosuppressive therapy. We investigated the outcome of COVID-19 infections in hospitalized transplant patients and autoimmune immunosuppressed patients.
Methods: This is a retrospective chart review of outcomes for adult patients admitted to our institution with COVID-19 infection from March 2020 to September 2021 on immunosuppressive drugs. Patients were categorized into either a transplant or ARD group. Baseline characteristics, comorbidities, and severe outcomes during admissions were evaluated. Chi2 tests were used to compare outcomes. Odds ratios were adjusted for age, sex, and race.
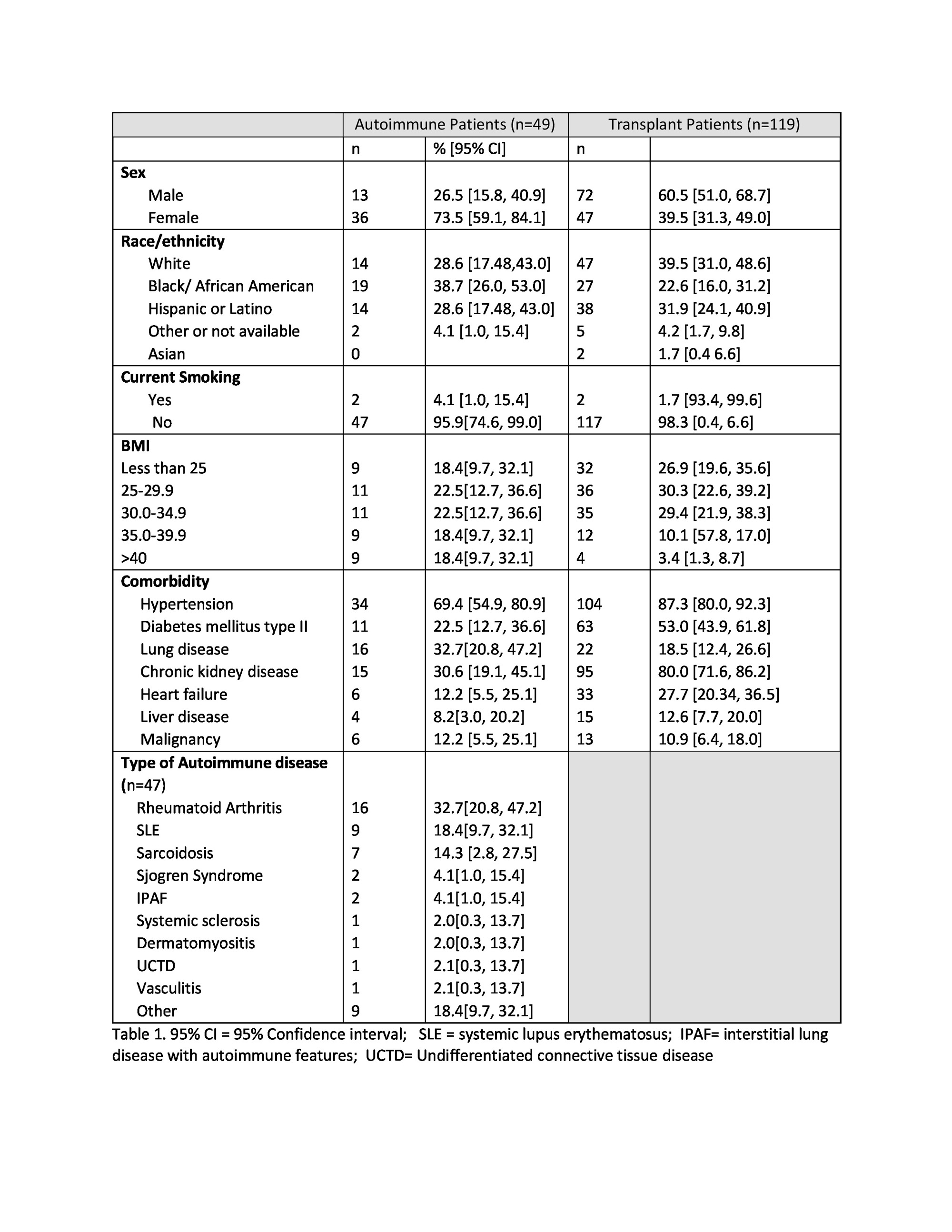
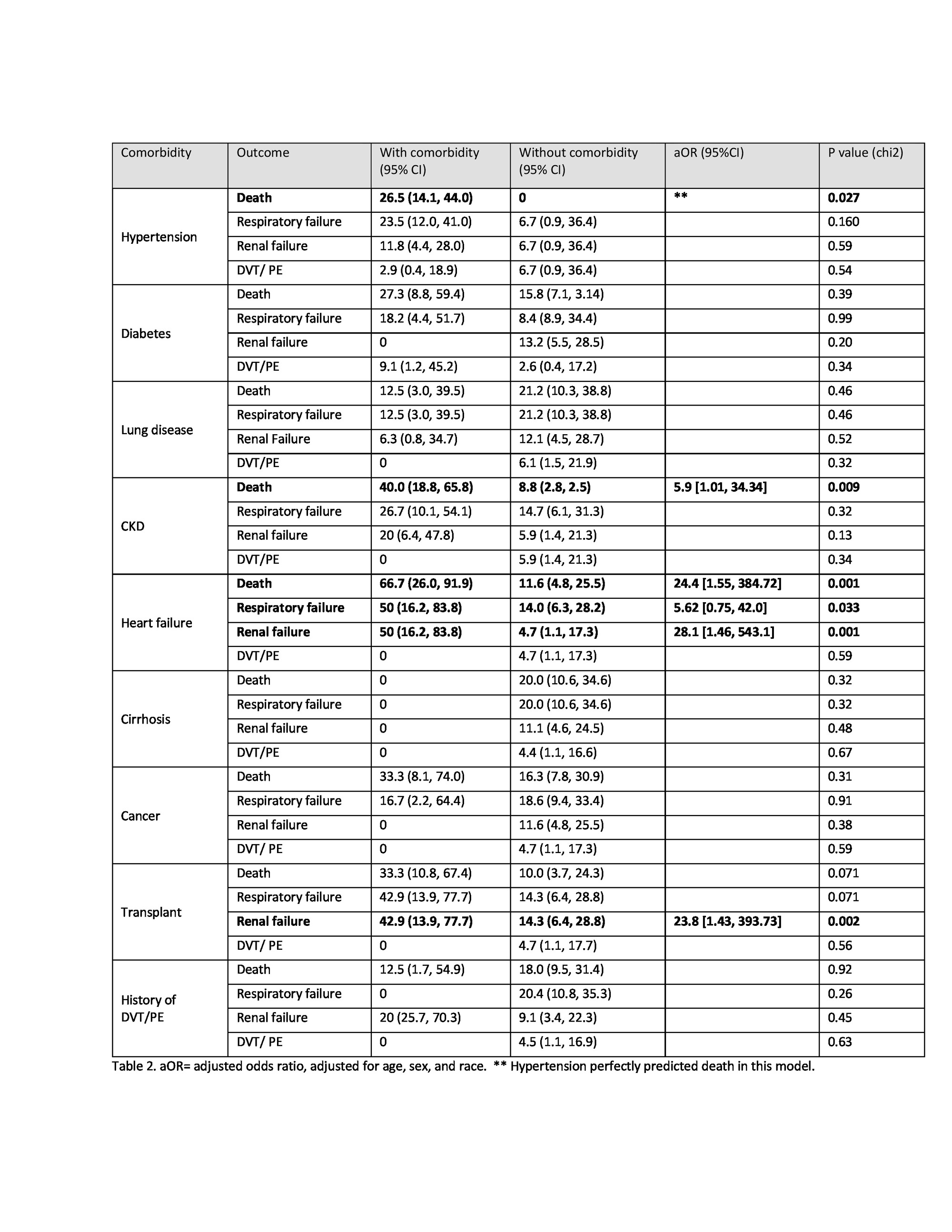
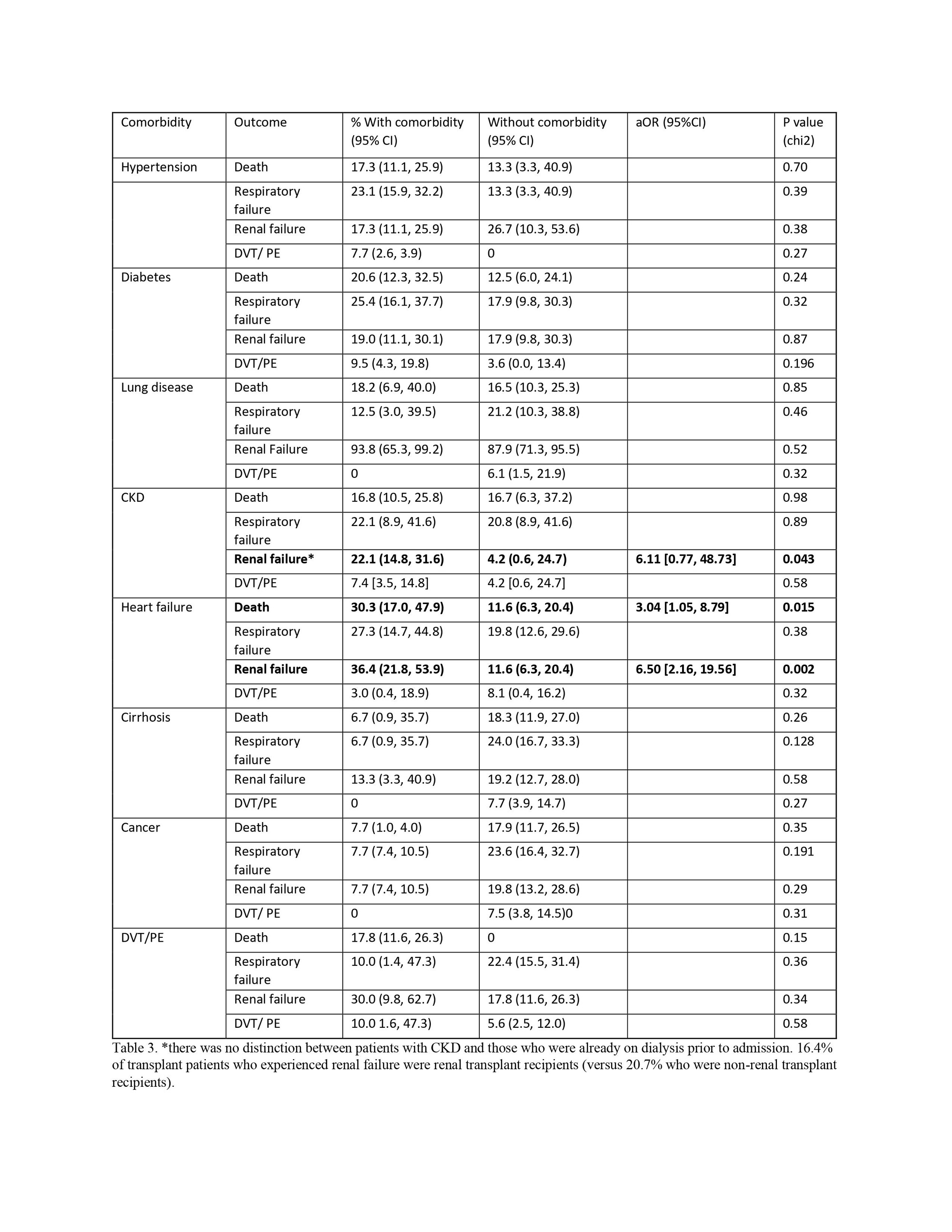
Results: Of 2,140 cases reviewed, 49 patients with ARD requiring immunosuppression and 119 transplant patients were identified. The ARD group had a higher proportion of females than the transplant group (Table 1). More transplant patients had hypertension, diabetes mellitus, or chronic kidney disease (CKD). In the ARD group, 4.1% were current smokers, but seven patients (43.8%) with any history of smoking died compared with 2 (6.0%) non-smokers, although the adjusted odds ratio did not reach significance. The most common ARD was RA. Among 9 ARD patients who died, 3 had RA and SLE each. The mean age of ARD patients who died was 65.2 years. ARD patients with renal and respiratory failure were more likely to die than those without these adverse events (Table 2). Comorbidities with significantly increased risk of death in ARD patients were hypertension, CKD, and heart failure (Table 2). A history of heart failure or transplant was also associated with respiratory and renal failure. In the transplant group, a history of heart failure was associated with death, and patients with a history of CKD or heart failure were more likely to develop renal failure (Table 3). When comparing death, renal or, respiratory failure and thromboembolic events between transplant and ARD patients, there was an increase in renal failure for transplant patients compared to ARD patients (17.0 versus 4.8%, p= .017). While 14.3% of ARD patients and 16.9% of transplant patients died, and 21.8% of transplant patients required intubation, compared to 14.3% of ARD patients, these trends did not reach statistical significance. In transplant patients who died during their admission, the most common organ transplant was heart (22.7%) followed by kidney and lung (18 and 15%).
Conclusion: Studies have evaluated risk factors for severe COVID-19 outcomes in immunosuppressed patients, but there is limited literature comparing autoimmune disease and transplant patients that also evaluate severe outcomes such as renal failure and thromboembolic events. Besides renal failure, severe outcomes from COVID-19 were not significantly different between ARD and transplant patients. Risk factors for death, however, did differ between these groups. This study gives further insight into similarities and differences of immunosuppression’s impact on COVID-19 outcomes in autoimmune and transplant patients.
To cite this abstract in AMA style:
KC Y, Ostrowski R. Outcomes of COVID-19 Infection in Hospitalized Autoimmune Patients and Transplant Patients on Immunosuppression [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-hospitalized-autoimmune-patients-and-transplant-patients-on-immunosuppression/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-hospitalized-autoimmune-patients-and-transplant-patients-on-immunosuppression/