Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Assembling large cohorts of patients with rare diseases is difficult and limits the power to assess outcomes in systemic sclerosis (SSc) studies. Treatment in SSc varies significantly and is tailored to a patient’s disease manifestations. To investigate this variability, we identified a cohort of SSc patients in the EHR to examine real-world disease presentations and treatment practices.
Methods: We analyzed data from a de-identified EHR that contains over 3 million subjects with longitudinal clinical data. We identified potential SSc patients using a previously validated algorithm requiring ³ 4 SSc ICD-9 (710.1) or ICD-10-CM codes (M34.0, M34.1, M34.8, M34.9). We performed chart review to determine case status, disease manifestations, autoantibodies, and medication use. Patients were confirmed to have SSc if diagnosed by a rheumatologist, pulmonologist, or dermatologist. Disease manifestations were included if documented in inpatient or outpatient notes. Immunosuppressants and medications for gastroesophageal reflux disease (GERD), Raynaud’s phenomenon, and pulmonary hypertension (PH) were assessed through inpatient and outpatient notes and counted if ever used.
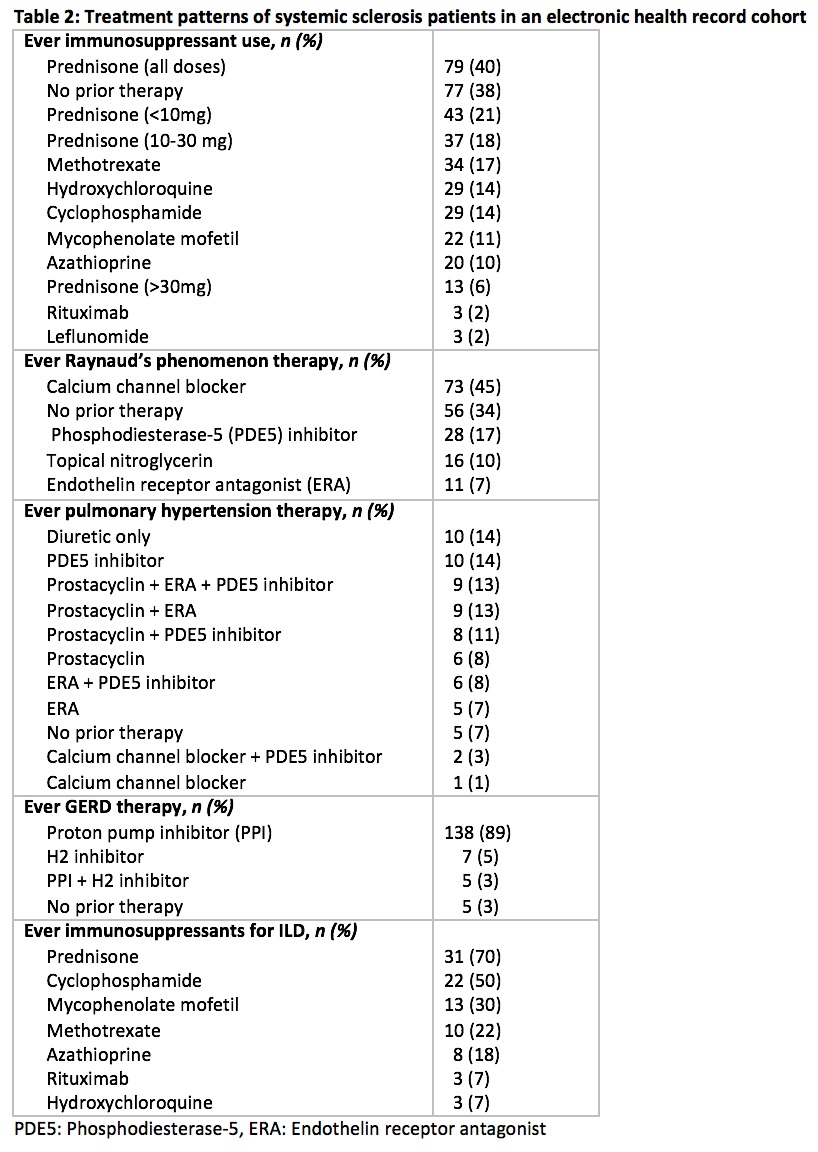
Results: Results: Of 223 patients identified by the algorithm, 196 were confirmed on chart review as SSc patients with an additional 4 mixed connective tissue disease patients. Of these 200, patients were predominantly female (84%) and Caucasian (87%) (Table 1). Of patients with available tests, 95% had a positive antinuclear antibody (titer ≥ 1:160). Most were of the limited cutaneous subtype (83%). Overall, 22% had interstitial lung disease (ILD), 36% PH, and 3% renal crisis. The most common disease manifestations were Raynaud’s phenomenon (82%) and GERD (78%). Of the patients with Raynaud’s phenomenon, 45% were ever on a calcium channel blocker and 34% were not on any medications (Table 2). Almost all patients with GERD were on acid suppression therapy (97%) with 89% on a proton pump inhibitor. Overall, immunosuppressant use varied widely, with the most commonly used medications being prednisone at any dose (40%) and methotrexate (17%). Only 16% of patients on prednisone were on doses higher than 30 mg daily, and a majority (69%) had co-existing ILD or arthritis. For the ILD patients, 91% were on immunosuppressants with the most frequently used medications being prednisone (70%) and cyclophosphamide (50%). Of the PH patients, 79% were on disease specific treatment with 21% not on therapy or on diuretics alone. A majority (60%) of the PH patients were managed with combination therapy.
Conclusion: We identified a large, real-world EHR cohort of SSc patients. The majority of SSc patients were on medications for GERD, PH, and ILD. This trend may reflect our EHR cohort being based at a tertiary care center with access to multi-disciplinary care. Despite high percentages of treatment, immunosuppressant treatments and medications for ILD and PH varied significantly between patients. In future studies, we will evaluate how real-world management and treatment practices impact clinical outcomes in SSc.
To cite this abstract in AMA style:
Kidwell K, Crofford L, Barnado A. Organ Specific Treatment Patterns of a Real-World, Electronic Health Record Cohort of Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/organ-specific-treatment-patterns-of-a-real-world-electronic-health-record-cohort-of-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/organ-specific-treatment-patterns-of-a-real-world-electronic-health-record-cohort-of-patients-with-systemic-sclerosis/