Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with rheumatic diseases commonly experience oral health issues such as dental caries, xerostomia, and periodontal disease. These complications are linked to both the disease itself and immunosuppressive treatments, often leading to reduced quality of life and poor systemic inflammatory control. Despite this, oral health remains insufficiently addressed in rheumatologic care.This study presents the experience of an interdisciplinary rheumatology-dentistry clinic. It evaluates the impact of collaborative care on early oral risk detection, health promotion, and oral health-related quality of life in patients with rheumatic diseases.
Methods: A structured interdisciplinary care model was established in 2017 to link rheumatologists with dental professionals. Its aim was to prevent oral health deterioration in patients with rheumatic diseases. During routine evaluations, rheumatologists screened for oral risk factors and referred patients to dentists trained in rheumatologic oral conditions.Dentists conducted comprehensive evaluations including physical exams, salivary tests, ICDAS (International Caries Detection and Assessment System), and GOHAI (Geriatric Oral Health Assessment Index) scoring. Individualized prevention plans were developed addressing hygiene, diet, salivary stimulation, and fluoride use. Referrals to dental specialists were made as necessary. The model ensured continuous monitoring of clinical and patient-reported outcomes, creating a feedback loop to promote adherence and sustained care integration (Figure 1).
Results: A total of 415 patients with rheumatic diseases were included. The mean age was 52.27 ± 14.17 years; 91.1% were female, and 6.3% were pregnant. Diagnoses included rheumatoid arthritis (57.1%), systemic lupus erythematosus (17.1%), primary Sjögren’s syndrome (14.2%), and other conditions (11.6%).All patients attended the initial dental consultation; 90% were referred to other dental specialties. Prevalence of oral conditions included dental caries in 60.7%, reduced unstimulated salivary flow in 46.7%, and missing teeth in 10.3%. All received personalized oral health recommendations from trained dental professionals.Initially launched in collaboration with the dentistry department, the program expanded in 2024 due to increasing demand. That year, dental services were fully integrated within the rheumatology clinic’s physical space, significantly increasing dental consultations and improving referral pathways and specialized care access (Figure 2).
Conclusion: Integrating dental evaluations into rheumatology care improved detection and management of oral health issues in patients with rheumatic diseases. The increase in referrals and enhanced interdisciplinary collaboration demonstrates the feasibility and value of coordinated care. Immediate referrals and universal oral health guidance highlight the success of this patient-centered, integrated model.
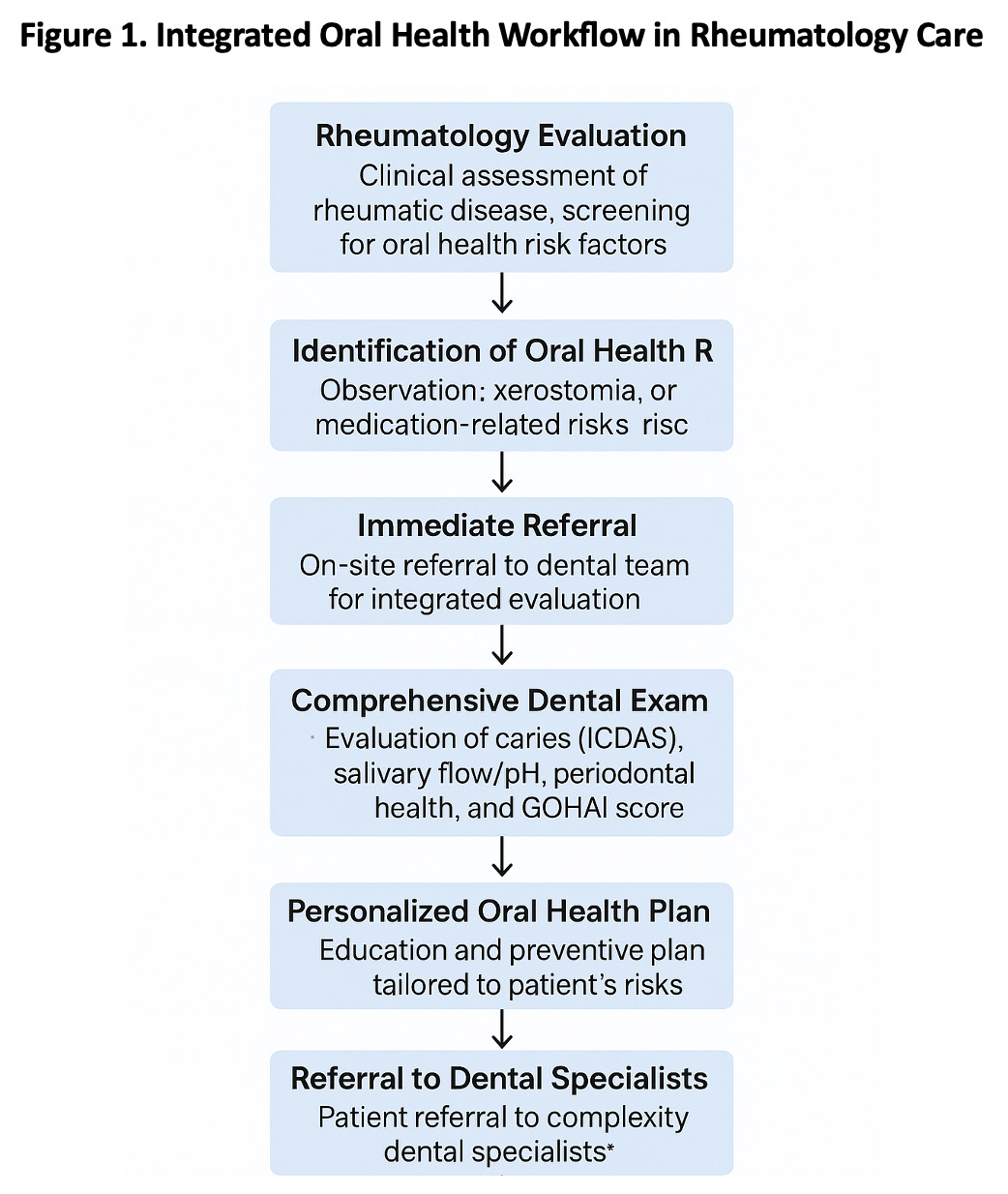 Figure 1. Integrated Oral Health Workflow in Rheumatology Care
Figure 1. Integrated Oral Health Workflow in Rheumatology Care
.jpg) Figure 2. Rheumatologic and dental assessments over time in patients with rheumatic diseases reporting altered oral health perception (April 2021 – April 2025).
Figure 2. Rheumatologic and dental assessments over time in patients with rheumatic diseases reporting altered oral health perception (April 2021 – April 2025).
To cite this abstract in AMA style:
Alarcon-Jarquin M, Garcia-Garcia F, Lopez-Flores V, Gonzalez-Melendez A, Figueroa-Parra G, Galarza-Delgado D, Riega-Torres J. Oral Health in Patients with Rheumatic Diseases: A Pilot Quality Improvement Program [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/oral-health-in-patients-with-rheumatic-diseases-a-pilot-quality-improvement-program/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/oral-health-in-patients-with-rheumatic-diseases-a-pilot-quality-improvement-program/
