Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Current axial spondyloarthritis (axSpA) guidelines do not provide recommendations for opioids in pain management. Opioid use is common in axSpA, despite widespread uptake of effective biologic therapies. Using a US claims database, we examined temporal trends in prescriptions for opioids in conjunction with NSAIDs and TNFi between 2008-2021.
Methods: We identified a cohort of adults with radiographic axSpA (r-axSpA) in the Merative MarketScan database, aged 18-65 with continuous enrollment for ≥2 years, from 2006-2021. r-axSpA was defined by ≥2 ICD-9 or ICD-10 codes ≥7 days apart. We excluded patients with codes for rheumatoid arthritis or malignancy preceding r-axSpA diagnosis.
Patients were followed until codes for hospice/palliative care services, death, or the end of the study (12/2021). We extracted demographics and clinical characteristics including baseline treatments and comorbidities at baseline.
Prescription data was extracted for opioids (excluding methadone), NSAIDs, and TNFi. We calculated annual prescription rates for opioids and comparator drugs (NSAIDs and TNFi), as the number of prescriptions in a calendar year divided by person-time contributed by enrolled subjects meeting inclusion criteria for the year.
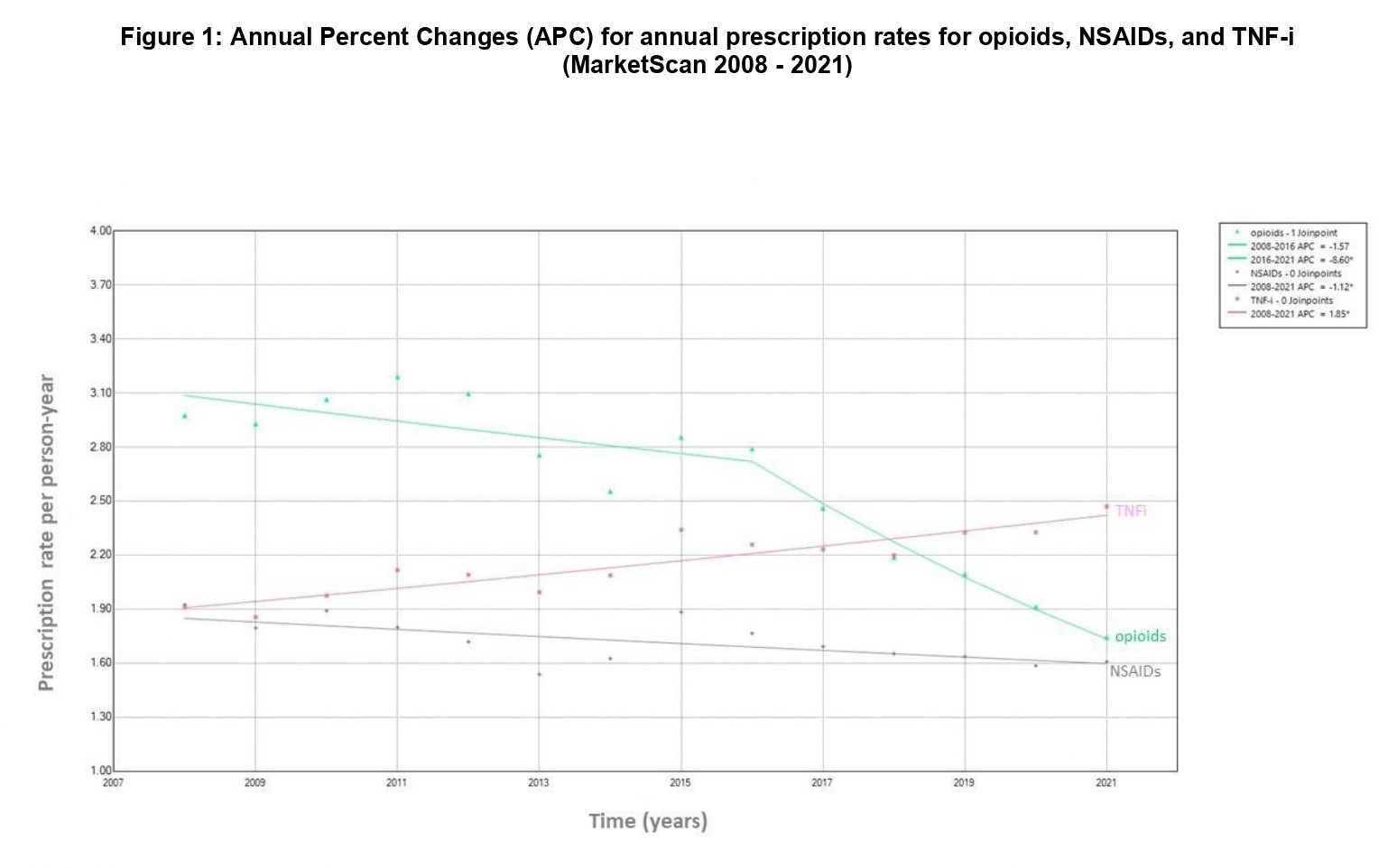
We analyzed trends in annual prescription rates using joinpoint regression analysis, following the method recommended by the National Cancer Institute. The number and locations of joinpoints in the data are identified by model fit and annual percent changes (APC) calculated for each segment.
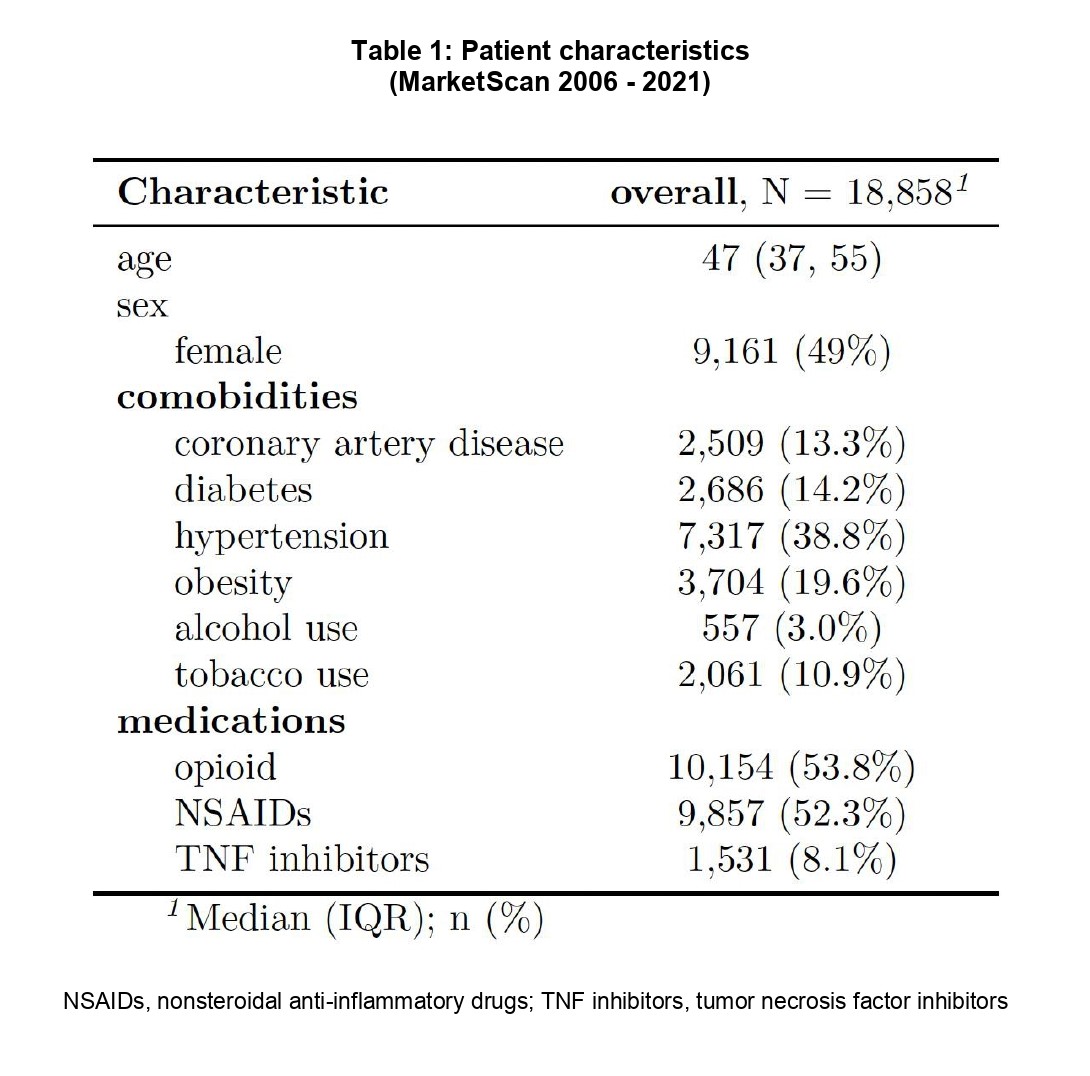
Results: We identified 18,858 individuals with incident r-axSpA (median age 47 years, 51% male). 2,509 (13.3%) had a history of coronary artery disease, and 1,624 (8.6%) had chronic kidney disease. Baseline csDMARD use was present in 13.6% and glucocorticoid use in 40.3% (Table 1).
Opioid prescription rates decreased by 1.5% annually (APC -1.5; 95% CI -3.0 – 1.7) in 2008-2016 and decreased by 8.6% annually (APC -8.6; 95% CI -14.5 – -5.7) in 2016-2021. NSAID rates decreased by 1.1% annually (APC -1.1; 95% CI -1.9 – -0.2) whereas TNFi rates increased by 1.8% annually (APC 1.8; 95% CI 1.2 – 2.4) in 2008-2021 (Figure 1).
Conclusion: In this US-based claims database, opioid prescription rates decreased with the rising uptake of TNFi along with decreased rates for NSAIDs. Findings may reflect secular changes in opioid prescribing for chronic non-cancer pain in the US, as well as improving axSpA management.
To cite this abstract in AMA style:
Degirmenci B, Peloquin C, Lodi S, Machado P, Jafarzadeh S, Neogi T, Gensler L, Dubreuil M, Liew J. Opioid Prescription Rates in Patients with Radiographic Axial Spondyloarthritis in the US Between 2008-2021: A Joinpoint Regression Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/opioid-prescription-rates-in-patients-with-radiographic-axial-spondyloarthritis-in-the-us-between-2008-2021-a-joinpoint-regression-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-prescription-rates-in-patients-with-radiographic-axial-spondyloarthritis-in-the-us-between-2008-2021-a-joinpoint-regression-analysis/