Session Information
Date: Wednesday, November 13, 2019
Title: 6W010: Pediatric Rheumatology – Clinical III: Juvenile SLE & Dermatomyositis (2864–2869)
Session Type: ACR Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: There is a need for clinically useful measures of cardiovascular (CV) risk in pediatric-onset SLE (pSLE). Nocturnal blood pressure (BP) non-dipping (loss of the physiologic nocturnal decline in BP) is a reversible marker of CV risk and potential treatment target that can be reproducibly measured by ambulatory blood pressure monitoring (ABPM). We assessed the frequency of non-dipping BP in pSLE and evaluated its association with vascular and cardiac function.
Methods: Twenty subjects 9-21 years of age with prevalent pSLE underwent comprehensive vascular testing, including 24-hour ABPM, peripheral endothelial function (EndoPAT), pulse wave velocity (PWV) for arterial stiffness, pulse wave analysis (PWA) for central BP, carotid ultrasound for intima-media thickness (cIMT), echocardiography for left ventricular (LV) strain and diastolic function, and fasting lipids. Additional clinical data was abstracted from charts, including longitudinal disease activity (SLEDAI-2K) scores. The primary outcome was prevalence of non-dipping (< 10% nocturnal decline in mean SBP or DBP). Secondary outcomes included prevalence of nocturnal and masked hypertension, defined by BP load (% of readings >95th%ile). We used descriptive statistics to assess patient characteristics in dippers and non-dippers. We used Pearson or Spearman rank correlation tests to evaluate relationships between SBP/DBP dipping, BP load and vascular measures.
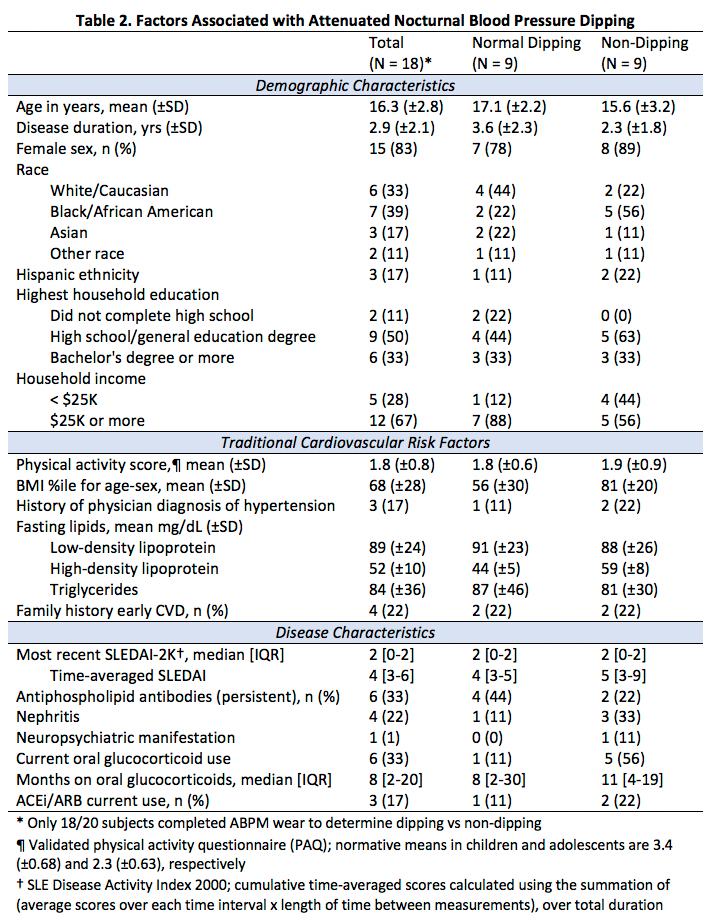
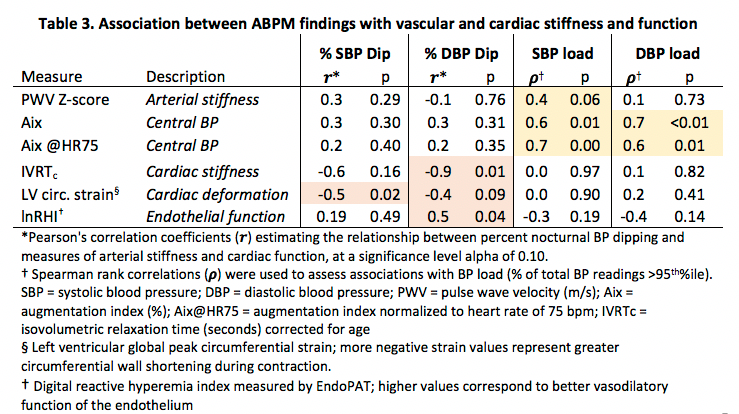
Results: The majority of subjects had inactive disease at the time of assessment (median SLEDAI 2 [interquartile range 0-2]), with a mean disease duration of 2.9 years (±2.1). 18/20 ABPM studies were evaluable. Agreement between hypertension category by manual office BP and 24-hour ambulatory mean SBP/DBP was poor (kappa 0.08). The prevalence of non-dipping and nocturnal hypertension was 50% and 11%, respectively, which occurred even in the absence of white coat or masked hypertension (Table 1). Compared to subjects with normal dipping, non-dippers were more often from low-income households and still using glucocorticoids. They also tended to have higher body mass index and time-averaged cumulative disease activity (Table 2). Reduced SBP/DBP dipping correlated with poorer endothelial function, decreased myocardial shortening (less negative strain) and increased LV stiffness (prolonged isovolumetric relaxation) (Table 3). In contrast, higher BP load was strongly correlated with increased arterial stiffness and central BP, but not with endothelial or cardiac function.
Conclusion: In a racially diverse group of children and adolescents with pSLE with low disease activity, there is a high prevalence of nocturnal BP non-dipping even in the absence of systemic hypertension. BP load relates to arterial stiffness, whereas nocturnal BP dipping relates to subclinical LV strain and endothelial function, and therefore ABPM abnormalities may represent two distinct mechanisms of early CV disease in pSLE. There is a potential role for routine ABPM in cardiovascular risk stratification of youth with pSLE.
This research was supported by the Lupus Foundation of America, Inc.
To cite this abstract in AMA style:
Chang J, Goldberg T, McGuire S, Waqar L, Meyers K, Mercer-Rosa L, Weiss P, Knight A. Nocturnal Blood Pressure Dipping as a Marker of Endothelial and Cardiac Function in Pediatric-onset Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/nocturnal-blood-pressure-dipping-as-a-marker-of-endothelial-and-cardiac-function-in-pediatric-onset-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nocturnal-blood-pressure-dipping-as-a-marker-of-endothelial-and-cardiac-function-in-pediatric-onset-systemic-lupus-erythematosus/