Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Thursday, April 30, 2020
Title: Poster Session 1
Session Type: ACR Abstract Session
Session Time: 6:00PM-7:00PM
Background/Purpose: Missed ambulatory visits, or “no-shows,” limit patient access, increase costs, occupy provider time, and lead to worse patient outcomes. Only a few studies have been done in pediatric subspecialties. To our knowledge, no studies on this subject have been performed in pediatric rheumatology. The demand for pediatric rheumatologists is high and access to care is limited. It would be beneficial to understand factors related to missed appointments in order to address these barriers. Prior studies in pediatric subspecialties and primary care have identified factors that include payor source, distance from clinic, and lag time. Here we explore these factors and other reasons in our own clinic population based on show rate.
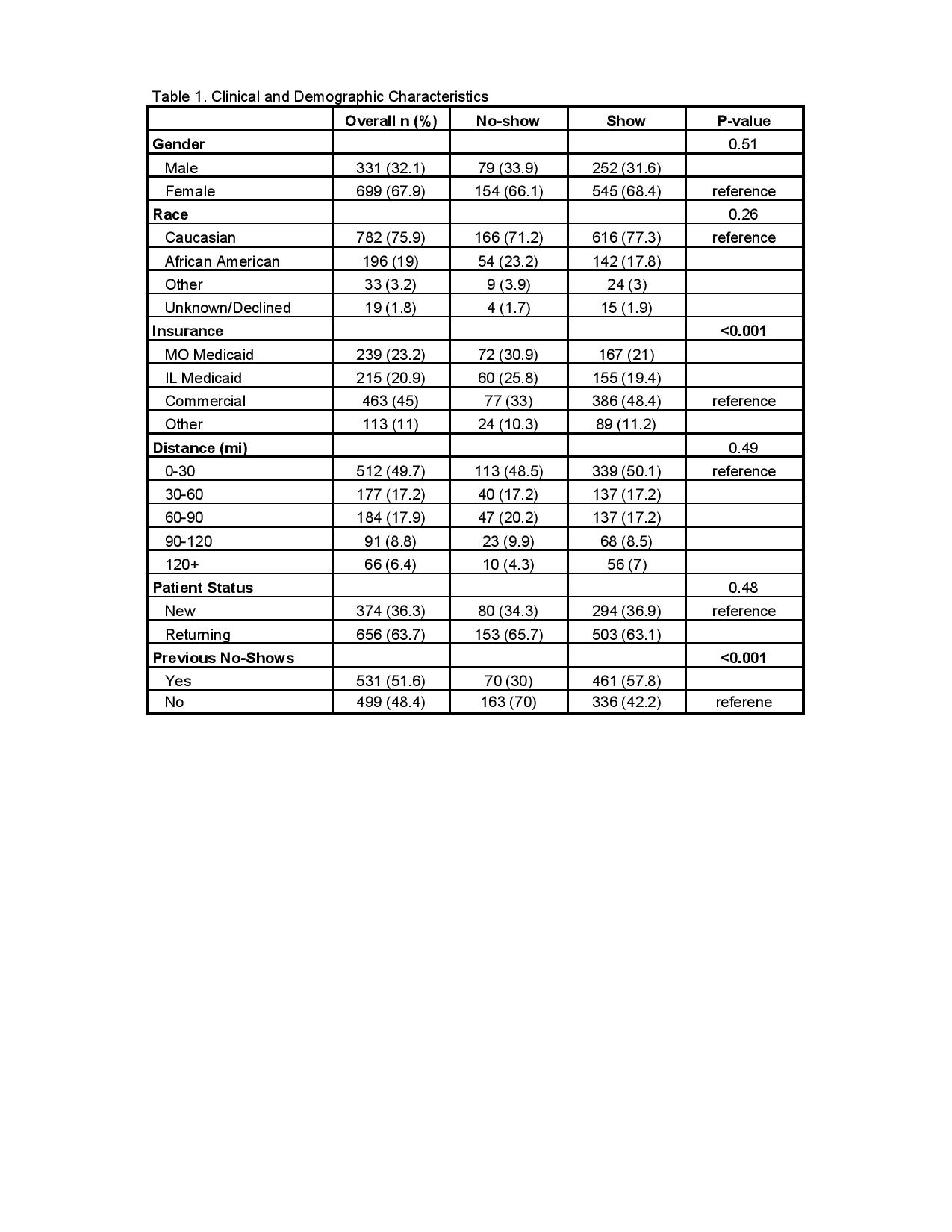
Methods: A retrospective chart review of each missed and arrived appointment in a single provider’s clinic was conducted at the SSM Health Cardinal Glennon Children’s Hospital in Saint Louis, Missouri between July 2016 and October 2018. Information obtained was race, gender, date (season and month), the day of the week, history of no-show, time of appointment, appointment type (new patient or follow-up), and payor source. Chi-square tests were utilized to examine differences between show and no-show groups on categorical variables.
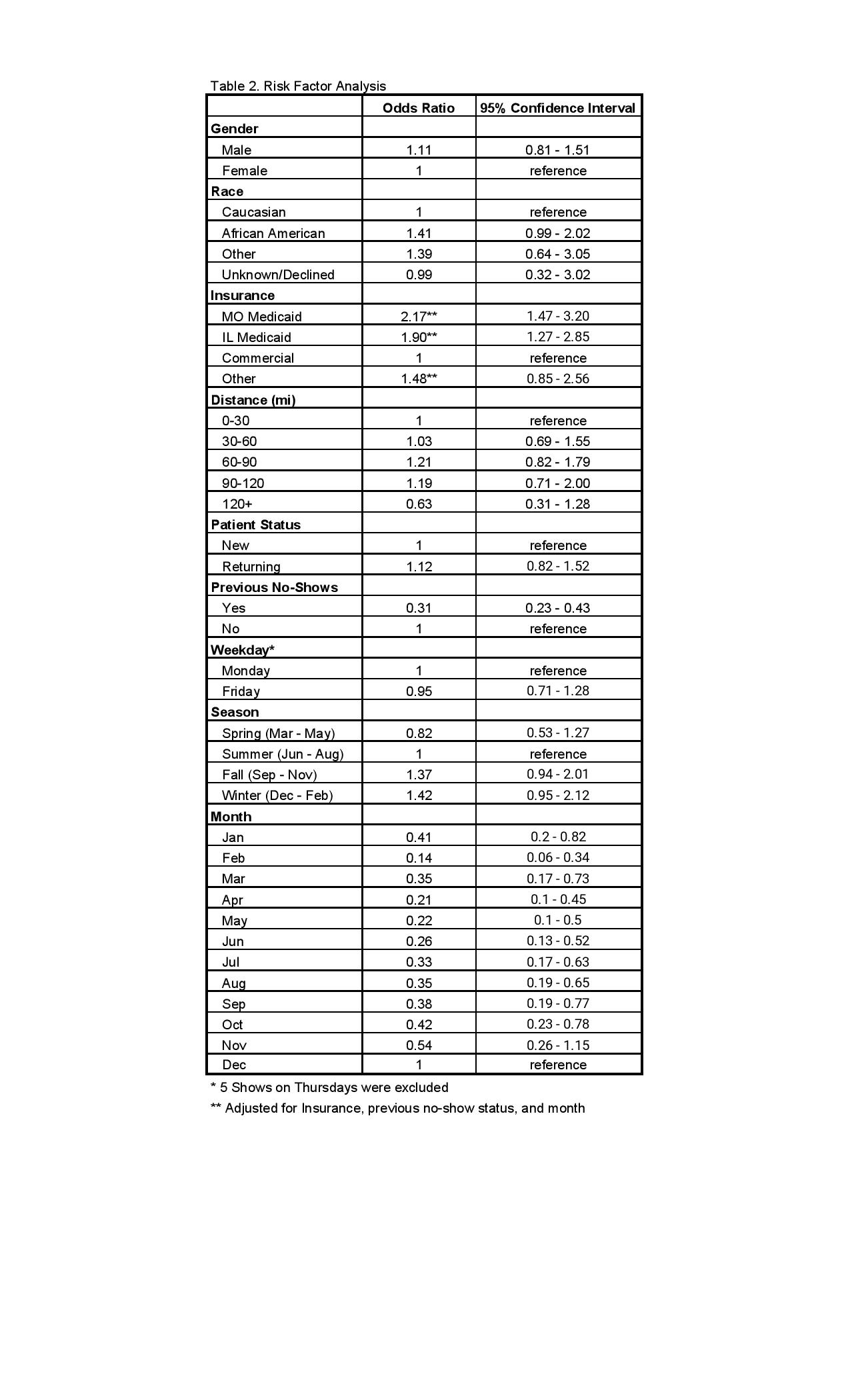
Results: Overall, 22.6% of patients missed their appointments. Patients with Missouri (MO) and Illinois (IL) Medicaid were more likely to miss appointments (MO, OR 2.16; IL, OR 1.94) than patients who held commercial insurance or other insurance types (p < 0.001). Patients with previous no-shows were significantly more likely to make appointments than those who did not have previous no-shows (OR 0.31) (p < 0.001). Differences in distance from the clinic (p = 0.49), patient status, (p = 0.48), day of the week (p = 0.75), gender (p = 0.51), season, and race (p = 0.26) were not found to be significant. (Tables 1&2)
Conclusion: Missed appointments serve as a major challenge in healthcare, especially in pediatric rheumatology where the number of specialized physicians remains relatively low in a field of high demand. We sought to identify the factors that contribute to missed appointments in our own clinic, hoping to further understand how to mitigate these factors. Through our analysis, payor source was the only significant factor that correlated with no-show rate. Patients with MO and IL Medicaid were significantly more likely to miss appointments compared to those with commercial insurance. Contrary to what we had expected, patients who had previous no-shows were more likely to make appointments. Other factors that we considered, including race, gender, day of the week, and patient status, were not found to be statistically significant. Our study was not without limitations. There are other socio-economic characteristics that are difficult to obtain that may be associated with barriers to care. We also did not factor in the diagnosis or severity of disease, which could possibly affect show rates. Additional investigation into these barriers is needed to fully understand missed visits. Overall, the data from the study suggests that interventions targeting patients with Medicaid, and identifying other modifiable factors could influence no-show rate.
To cite this abstract in AMA style:
Ong S, Li X, Dalrymple A. No-Shows: a Search for Modifiable Risk Factors [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/no-shows-a-search-for-modifiable-risk-factors/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/no-shows-a-search-for-modifiable-risk-factors/