Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Some previously published studies suggest that patients with rheumatoid arthritis (RA) are at an increased risk of developing diabetes mellitus. We examined the risk of incident type 2 diabetes mellitus (T2DM) among RA patients compared to four non-RA comparison cohorts.
Methods: Using a large US commercial insurance database, Optum Clinformatics (2005-2017), we identified RA patients based on ≥2 diagnosis codes for RA and use of ≥1 disease-modifying antirheumatic drugs (index date). We selected four comparison cohorts with ≥2 disease-specific diagnosis codes and ≥1 dispensing of disease-specific drugs: 1) general non-RA patients, 2) hypertension, 3) osteoarthritis (OA), and 4) psoriatic arthritis (PsA) patients as an inflammatory arthritis comparison cohort. All study patients were ≥18 years old with 365 days of continuous enrollment prior to the index date. Patients with diabetes diagnosis or use of any anti-diabetic drugs at baseline were excluded. We also excluded patients with RA or PsA from the non-RA, non-PsA cohorts. RA patients were matched to comparator cohorts (except PsA) with age, sex, and index date. Incidence T2DM was defined as a diagnosis of T2DM plus a new dispensing of anti-diabetic drugs within +/- 30 days. Patients were followed up from the day (for the primary analysis) or one year (for the secondary analysis to minimize surveillance bias) after the index date to the earliest event of: 1) occurrence of T2DM, 2) disenrollment, 3) end of data, 4) death, or 5) occurrence of RA or PsA in other cohorts. We used multivariable Cox-proportional hazards model to estimate hazard ratios (HR) of incident T2DM among RA versus each of comparison cohorts, accounting for >40 baseline covariates including demographics, co-morbidities, co-medications, lab ordered, and healthcare utilizations. To validate our results, we selected hip fracture as a positive control outcome since RA is known to increase the risk of hip fracture.
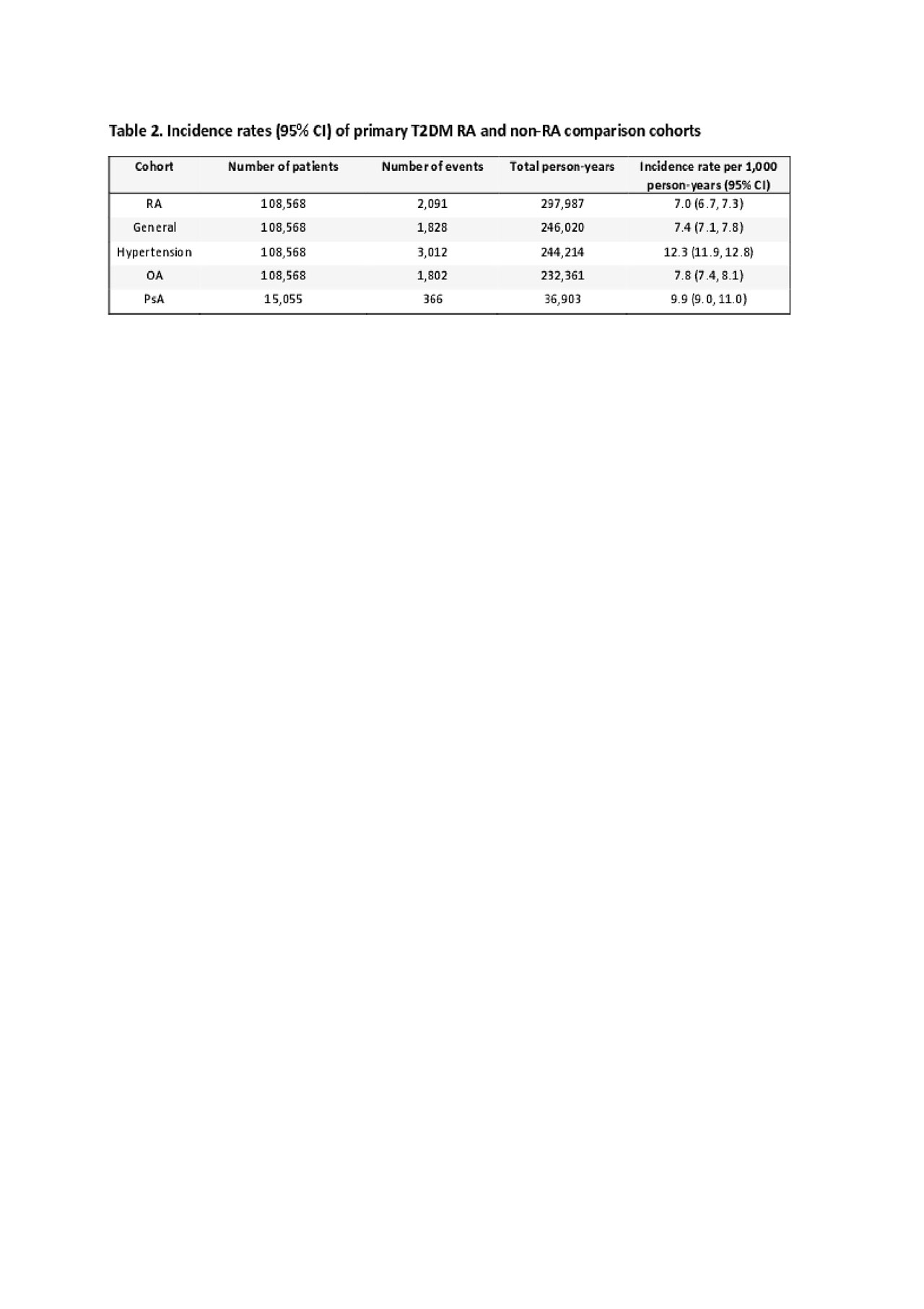
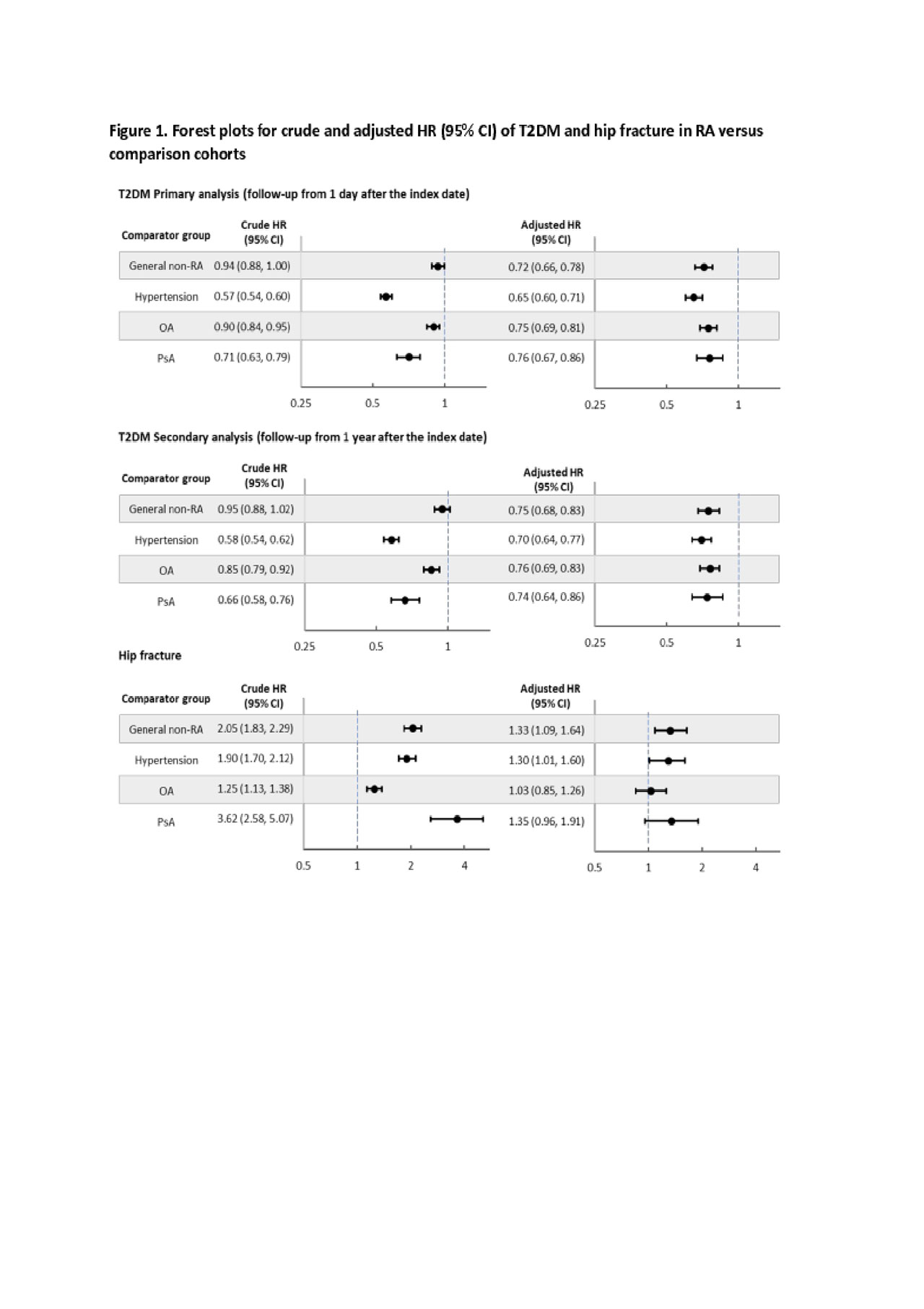
Results: A total of 108,568 RA patients were 1:1 matched to the hypertension, OA, and general non-RA cohorts on age, sex, and index date. 15,055 of PsA patients were identified. Mean age was 55.6 years among RA/general non-RA/hypertension/OA cohort and 77.3% were female. PsA patients had a mean age of 48.6 years and 48.6% were female (Table 1). During the mean 2.4 years of follow-up, we observed 2,091 incident T2DM events in RA patients, 1,828 in the general non-RA cohort, 3,012 in hypertension, 1,802 in OA, and 366 in PsA cohort. The crude incidence rate of T2DM was the lowest in the RA cohort (7.0 per 1,000 person-years) and highest (12.3 per 1,000 person-years) in the hypertension cohort (Table 2). After adjusting for baseline covariates, RA was associated with a 24-35% lower risk of incident T2DM compared to the comparison groups (Figure 1). The secondary analysis showed consistent results. Our positive control outcome analysis showed over 30% increased risk of hip fracture in RA patients compared to the general non-RA, hypertension, and PsA patients (Figure 1).
Conclusion: In this large cohort study with over 10 years of study period, RA patients had a lower rate of incident T2DM compared to the general non-RA, hypertension, OA, and PsA cohorts.
To cite this abstract in AMA style:
Jin Y, Chen S, Liu J, Desai R, Kim S. No Increased Risk of Incidence Diabetes in Patients with Rheumatoid Arthritis Compared to Patients Without RA [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/no-increased-risk-of-incidence-diabetes-in-patients-with-rheumatoid-arthritis-compared-to-patients-without-ra/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/no-increased-risk-of-incidence-diabetes-in-patients-with-rheumatoid-arthritis-compared-to-patients-without-ra/