Session Information
Date: Sunday, November 12, 2023
Title: (0380–0422) RA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is associated with a 2-fold higher risk of venous thromboembolism (VTE) compared with the general population. The immune system and hemostatic system are closely linked by a shared origin. Inflammation affects thrombotic responses by upregulating procoagulants and downregulating anticoagulants and fibrinolysis. Tumor necrosis factor (TNF), an important mediator in the inflammatory pathway, induces a disbalance between the coagulation system and fibrinolytic system, resulting in a hypercoagulable state. In addition, several studies have suggested that some Janus kinase-inhibitors (JAKi) might be associated with an increased risk for VTE. However, the underlying pathogenic mechanisms have yet to be elucidated. Our objective was to compare changes in hemostatic parameters during treatment with TNF-blockers and JAKi in RA.
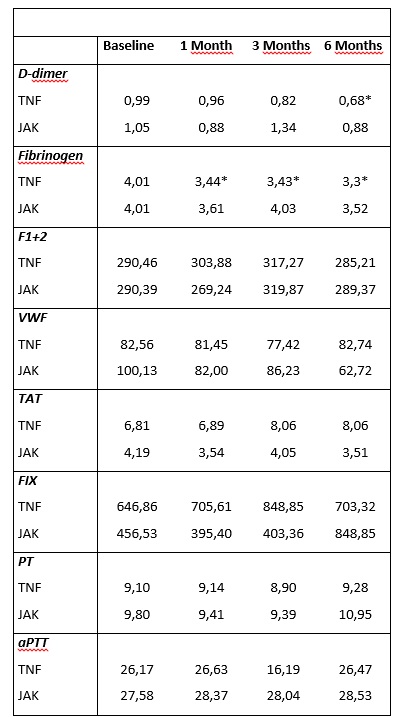
Methods: Biomarkers for the coagulation system, including D-dimer, fibrinogen, PT, aPTT, F1+2, TAT, F IX and vWF, were prospectively measured in 121 consecutive RA patients: 83 patients treated with aTNF and 38 patients with JAKi. Data were collected at baseline, after 1, 3, and 6 months.
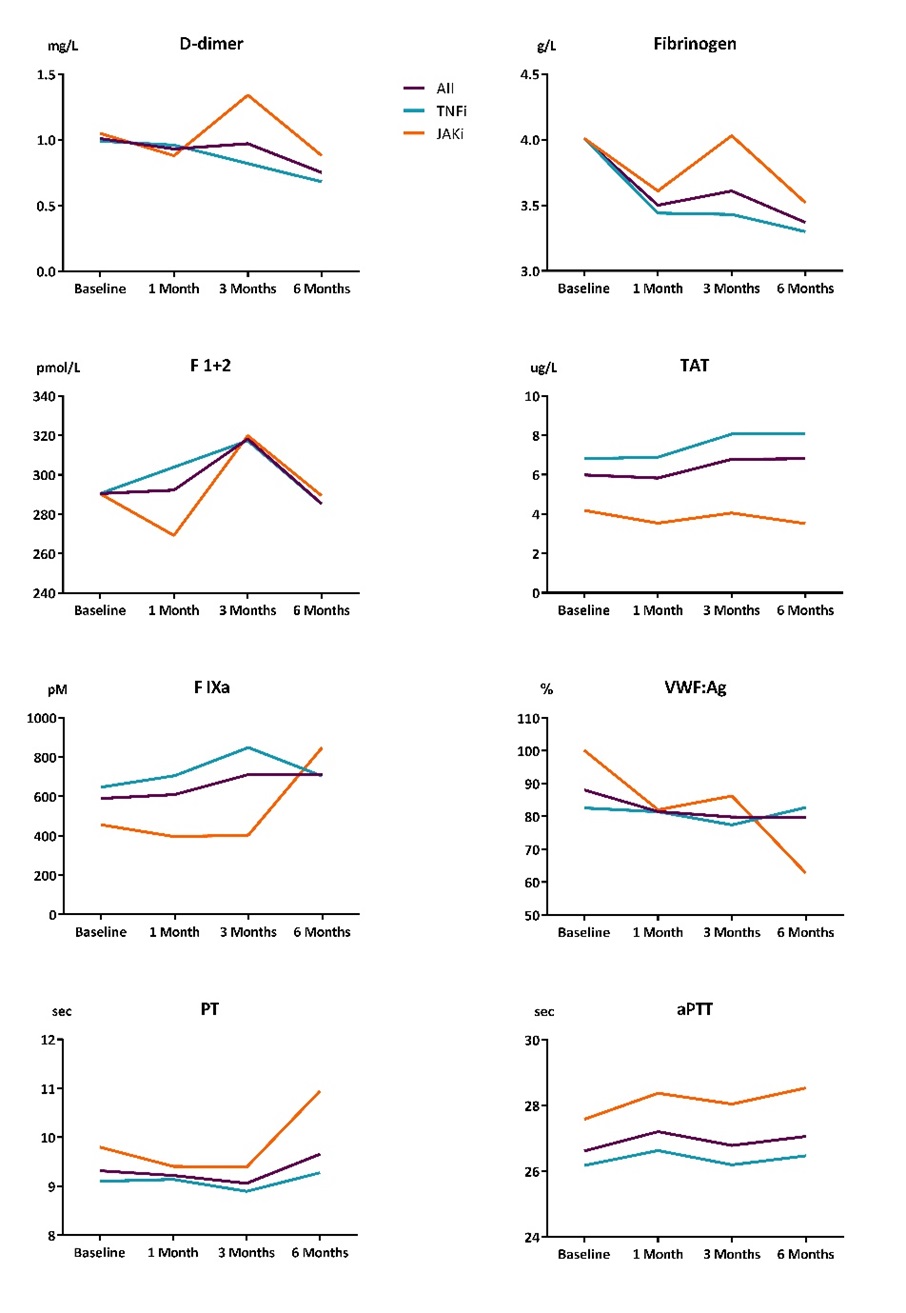
Results: Mean age for all patients was 57 (±14) years, 76% were female. Mean DAS28-CRP at baseline for TNF-inhibitor group was 3.6 (±1.3) and 4.1 (±1.4) for JAKi group, steadily declining in aTNF users, while decreasing in JAKi users with an intermittent peak at 3 months. Baseline coagulation markers levels were comparable between the groups. D-dimer and vWF levels were slightly higher in the JAKi group (p = 0.30 and p = 0.08, respectively), while F IXa levels were lower (p = 0.17). D-dimer and fibrinogen levels steadily declined in the aTNF group, while fluctuating in the JAKi group, with a peak at 3 months with a subsequent decline thereafter (Figure 1). In aTNF users, TAT increased slightly during follow-up. VWF, PT and aPTT remained relatively stable, while F IXa and F 1+2 showed an increase after 3 months of follow-up, after which they returned to baseline. In JAKi users, D-dimer, fibrinogen, VWF and F 1+2 fluctuated, with a peak after 3 months and then a subsequent decline. F IX and PT initially decreased slightly but increased steadily after 6 months, while TAT and aPTT remained stable during follow-up.
Conclusion: The pro-thrombotic tendency in active RA declined during effective treatment with both aTNF as well as JAKi. A gradually decrease in D-dimer and fibrinogen was seen after 6 months of treatment. The transient increase of coagulation activation in JAKi users at three months coincided with increased disease activity. Altogether, our data suggests that an increased VTE risk in the first six months due to wither treatment aTNF or JAKi seems unlikely. Whether or not the risk increases beyond this time period remains to be investigated.
To cite this abstract in AMA style:
Hansildaar R, Raadsen R, Heslinga M, Nurmohamed M. No Clinically Relevant Changes in Coagulation Activation Between Patients Initiating TNF-blockers versus JAK-inhibitors [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/no-clinically-relevant-changes-in-coagulation-activation-between-patients-initiating-tnf-blockers-versus-jak-inhibitors/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/no-clinically-relevant-changes-in-coagulation-activation-between-patients-initiating-tnf-blockers-versus-jak-inhibitors/