Session Information
Date: Monday, November 14, 2016
Title: Miscellaneous Rheumatic and Inflammatory Diseases - Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Neuromyelitis optica (NMO) is an immune-mediated inflammatory disorder of the central nervous system that has been associated with systemic autoimmunity often cared for by rheumatologists. We examined whether clinical characteristics and treatments differed among patients with NMO treated by rheumatologists compared to non-rheumatologists.
Methods: We performed a retrospective cohort study using a large national health plan database from May 1, 2000 – June 30, 2013. Data collected included inpatient, outpatient, and pharmacy claims. Subjects were identified by having at least one International Classification of Disease, Ninth Revision, Clinical Modification (ID-9-CM) code for NMO, receipt of glucocorticoids, and an inpatient/acute care visit within 90 days of the index date (defined as the first documented code for NMO). Subjects <1 year of age and with ≥2 codes for multiple sclerosis were excluded. Subjects required continuous health plan enrollment for 6 months prior to and 12 months after the index date. The exposed group included subjects with ≥ 1 NMO diagnosis code documented by a rheumatologist. Systemic autoimmune conditions were identified by their respective ICD-9-CM codes. Pharmacy claims (via National Drug Code) were used to identify medication use. We were unable to reliably assess intravenous medications.
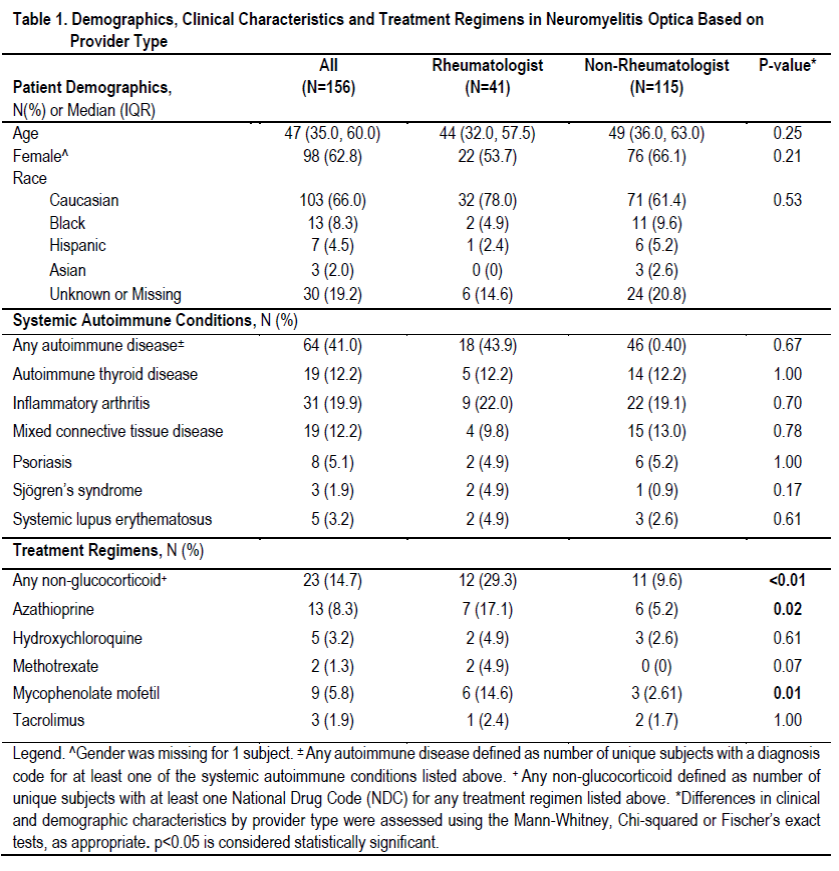
Results : 156 subjects met study criteria. Subjects were predominantly adult (90%), female (63%) and Caucasian (66%). Median age among the pediatric (<18 years old) group (N=15) was 12 years (IQR: 4-15) and among the adult cohort was 49 years (IQR: 38-64). 41% of subjects had at least one systemic autoimmune condition. A rheumatologist documented at least one NMO ICD-9-CM code for 27% of the subjects (N=41). Table 1 shows demographics, clinical characteristics and treatment regimens for subjects treated by a rheumatologist versus non-rheumatologist. There was no statistically significant difference in the proportion of subjects with a concomitant systemic autoimmune disease between the two groups (all p>0.05). Use of any non-glucocorticoid immunosuppressant was more common in the rheumatologist group (p<0.01). This finding persisted when restricted to the adult cohort (p<0.01) but was not true for the pediatric cohort (p=1.00). Azathioprine and mycophenolate mofetil were significantly more common in the rheumatologist group (p=0.02 and p=0.01, respectively). Methotrexate was more common among rheumatologists (4.9% vs. 0%) but was only marginally significant (p=0.07).
Conclusion: Patients with NMO cared for by a rheumatologist were more likely to receive non-glucocorticoid immunosuppressive agents. The most commonly used medications were azathioprine and mycophenolate mofetil. Future studies should address the use and effectiveness of non-glucocorticoid medications in the rheumatologic management of pediatric NMO.
To cite this abstract in AMA style:
Gmuca S, Xiao R, Waldman AT, Gerber JS, Weiss PF. Neuromyelitis Optica: Patient Characteristics and Treatment Patterns Among Rheumatologists Versus Non-Rheumatologists [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/neuromyelitis-optica-patient-characteristics-and-treatment-patterns-among-rheumatologists-versus-non-rheumatologists/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neuromyelitis-optica-patient-characteristics-and-treatment-patterns-among-rheumatologists-versus-non-rheumatologists/