Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Burnout, a syndrome of emotional exhaustion and depersonalization, adversely impacts healthcare and results in mood disturbances, poor patient and provider satisfaction and high turnover. Studies have shown burnout also plays a critical role in physician bias, with increased bias among those with higher rates of burnout. The SARS-CoV-2 pandemic increased levels of burnout and exposed the high prevalence of racial bias in healthcare. There is a critical need for methods to address burnout and bias in healthcare. Narrative medicine (NM) incorporates the stories of human experience into the medical realm and has been proven to strengthen relationships and increase empathy. To date, limited data investigating narrative medicine’s impact on burnout and bias has been promising. This pilot study aims to investigate the use of NM as a tool to address burnout and explore bias amongst a pediatric rheumatology division.
Methods: Physicians, nurses, medical assistants and staff at a single center enrolled in a series of six monthly 1-hour video-based sessions lead by co-facilitators (AL, and a NM-trained facilitator) after informed consent. Sessions utilized poetry, photography, paintings, and spoken word to inspire writing prompts around the medical experience. A Plan-Do-Study-Act approach was used to guide intervention adjustments based on participant post-session feedback. Demographics were collected, and standard surveys were administered at baseline, and after the third and sixth sessions, specifically: Mini Z Burnout, Copenhagen Burnout Inventory (CBI), Provider Health Questionnaire-9 (PHQ-9) as well as Implicit Association Testing (IAT) and explicit bias Feeling Thermometer (FT).Survey data were assessed for differences with a Wilcoxon signed rank test.
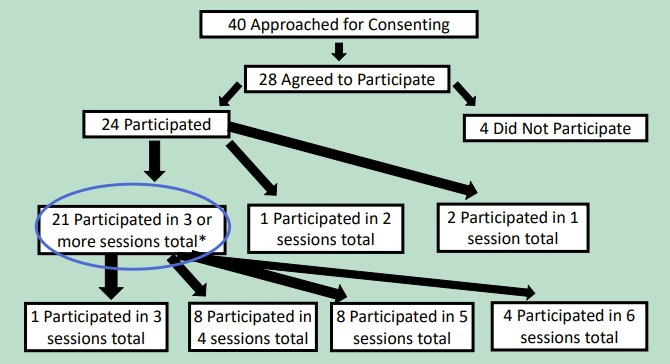
Results: Twenty-four participants with 21 females, 2 males and one non-binary were divided amongst 6 narrative medicine groups for the 6 total sessions. Data analysis was completed for those who attended 3 or more sessions (n=21) (See Figure 1). Self-identified race included 18 White, 4 Asian, 1 Black, and 1 who preferred not to answer. Participants included 8 attendings, 4 fellows, 2 nurses, 2 medical assistants, and 8 staff members. While no statistical significance was seen when evaluating questionnaires for the Mini Z Burnout, CBI, or PHQ-9 when comparing questionnaires from baseline and after 6 months into participation, there was a trend toward improvement with median CBI improved from 39.5 to 28.9, and median PHQ-9 score improved from 5 to 3. (Table 1). IAT showed a statistically significant shift towards positive association with African Americans following participation (p-value= 0.012), while FT showed a non-statistically significant explicit bias shift away from positive association with European Americans (p=0.096).
Conclusion: Narrative medicine is a feasible intervention that warrants further study as a means to address bias. Additional long-term analysis is needed to understand if these changes are durable.
To cite this abstract in AMA style:
Lanis A, Rosenwasser N, Morgan E. Narrative Medicine and Pediatric Rheumatology: Addressing Burnout and Bias [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/narrative-medicine-and-pediatric-rheumatology-addressing-burnout-and-bias-2/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/narrative-medicine-and-pediatric-rheumatology-addressing-burnout-and-bias-2/