Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular (CV) disease represents the leading cause of death in SLE. Traditional risk factors are less accurate at identifying cardiovascular risk in SLE than in the general population. N-Terminal pro-Brain Natriuretic Peptide (NT-proBNP) is a key biomarker to detect heart disease and predict cardiac outcomes, in non-lupus populations. We assessed NT-proBNP in a large cross-sectional sample of unselected SLE patients and investigated associations with CV damage.
Methods: Adults meeting ACR SLE classification have been consecutively enrolled in our Lupus Clinic cohort. Patients were followed yearly with evaluations of drugs, SLICC Damage Index (SDI), SLEDAI-2K, and other measures including cardiovascular risk factors. NT-proBNP (pg/mL) levels were measured in serum collected at annual research visits between March 2022 and April 2023. The main outcome was CV damage defined as any CV SDI events. Cross-sectional associations between NT-proBNP and this outcome were evaluated using multivariable logistic regression model.
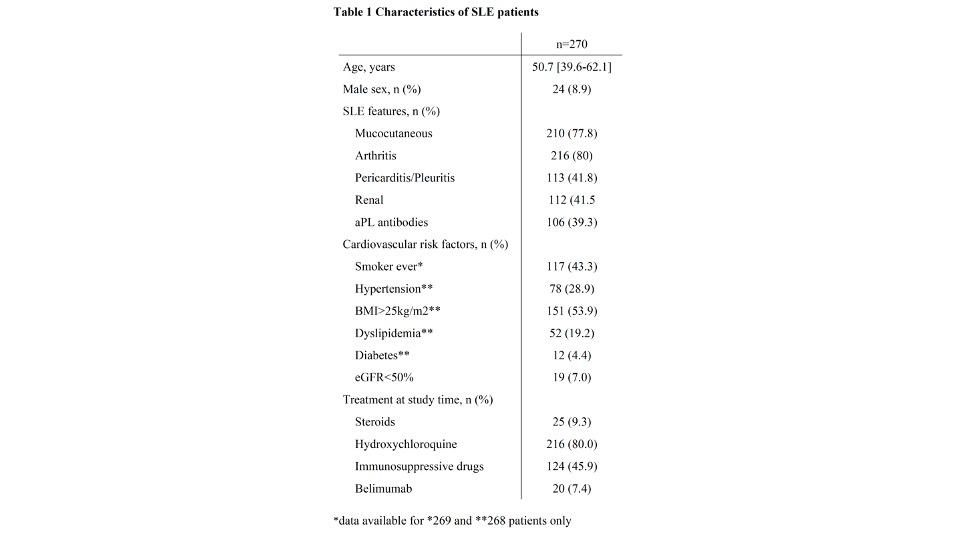
Results: Overall, 270 SLE patients (91% female 91%, median age of 50.7 [1st quartile- 3rd quartile: 39.6-62.1] years) from the MUHC cohort were included. At NT-proBNP assessment, median disease duration was 17.7 years [11.6-27.2] and median SLEDAI-2K and SDI scores were 2 [0-4] and 1 [0-3] respectively. Characteristics of patients are given in Table 1. Thirty-three (12%) patients had CV damage including coronary artery disease (n=14), cerebral vascular accident (n=12), chronic pericarditis (n=6), valvular diseases (n=5), cardiomyopathy (n=3) and peripheral artery disease (n=1). The median [1stquartile- 3rd quartile] NT–proBNP serum level was 95 [54-185] pg/mL. NT-proBNP levels were higher in patients with CV damage (281 [140-856] versus 84 [50-147] pg/mL in those without CV damage, P< 0.001) and were especially high in patients with more than one CV damage item (989 pg/mL [734–1725] versus 194 [122-327] pg/mL in those with one CV damage item only, P< 0.0001). The ROC curve for NT–proBNP demonstrated strong associations with CV damage (AUC 0.78, 95% CI 0.69-0.87). The threshold providing the best discrimination for those with/without CVD was 133 pg/mL, with a sensitivity of 79% (95% CI 64-91) and a specificity of 70% (95% CI 64-76). In multivariate analyses, hypertension (OR 3.3, 95% C 1.2-9.0), dyslipidemia (OR 3.6, 95% CI 1.3-9.6) and NT-proBNP >133 pg/mL (OR 7.0, 95% CI, 2.6-19.1) were strongly associated with CV damage. CV damage was less frequent in SLE patients on hydroxychloroquine (OR 0.3, 95% CI 0.1-0.8). Increased NT-proBNP levels were themselves associated with age (OR 4.2, 95% CI 2.2-8.3), smoking (OR 1.9, 95% CI 1.0-3.5), reduced eGFR (4.1, 95% CI 1.3-13.1), prior pericarditis/pleuritis (OR 2.5, 95% CI 1.4-4.5) and aPL antibodies (OR 2.6, 95% CI 1.4-4.9)
Conclusion: Serum NT-proBNP levels correlate with CV damage in SLE. Future evaluations are needed to identify the usefulness of NT-proBNP in tailoring treatments to prevent CV burden in SLE. The novel associations of NT-proBNP levels with pericarditis/pleuritis and aPL antibodies suggest new avenues for research to better understand what drives CV risk in SLE.
To cite this abstract in AMA style:
Sacre K, Vinet E, Pineau C, Mendel A, Kalache F, Grenier L, Huynh T, Bernatsky S. N-Terminal Pro-Brain Natriuretic Peptide Correlates Strongly with Cardiovascular Damage in Systemic Lupus Erythematous (SLE): A Cross-sectional Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/n-terminal-pro-brain-natriuretic-peptide-correlates-strongly-with-cardiovascular-damage-in-systemic-lupus-erythematous-sle-a-cross-sectional-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/n-terminal-pro-brain-natriuretic-peptide-correlates-strongly-with-cardiovascular-damage-in-systemic-lupus-erythematous-sle-a-cross-sectional-study/