Session Information
Date: Monday, November 8, 2021
Title: Epidemiology & Public Health Poster III: Other Rheumatic & Musculoskeletal Diseases (1022–1060)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with Systemic Lupus Erythematosus (SLE) have an increased burden of multimorbidity. Age is strongly associated with accumulation of comorbidities. Patients with SLE may experience multimorbidity at younger ages than their non-SLE controls due to exposure to toxic treatments, disease activity or accelerated aging. We aimed to compare multimorbidity among different age groups of patients with SLE and comparators without SLE.
Methods: We used the OptumLabs Data Warehouse (OLDW), a real-world data asset with de-identified administrative claims to identify cases of SLE and matched comparators. Cases were defined as patients with ≥3 diagnoses of SLE between 1/2006 and 9/2015. Comparators were persons without SLE matched 1:1 on age, sex, race/ethnicity, and enrollment date. Race was classified as White, Black, Asian and Hispanic. Multimorbidity (2 or more comorbidities) was defined using 172 chronic comorbidities from the chronic condition indicator of the clinical classification software (healthcare cost and utilization project). Two or more ICD-9 codes at least 30 days apart were used to define a comorbidity. SLE, cutaneous lupus, and rheumatoid arthritis codes were excluded from the analysis. A secondary analysis was performed including those with 5 or more comorbidities. Conditional logistic regression models were used to estimate odds ratios (OR) with 95% confidence intervals (CI) adjusted for region.
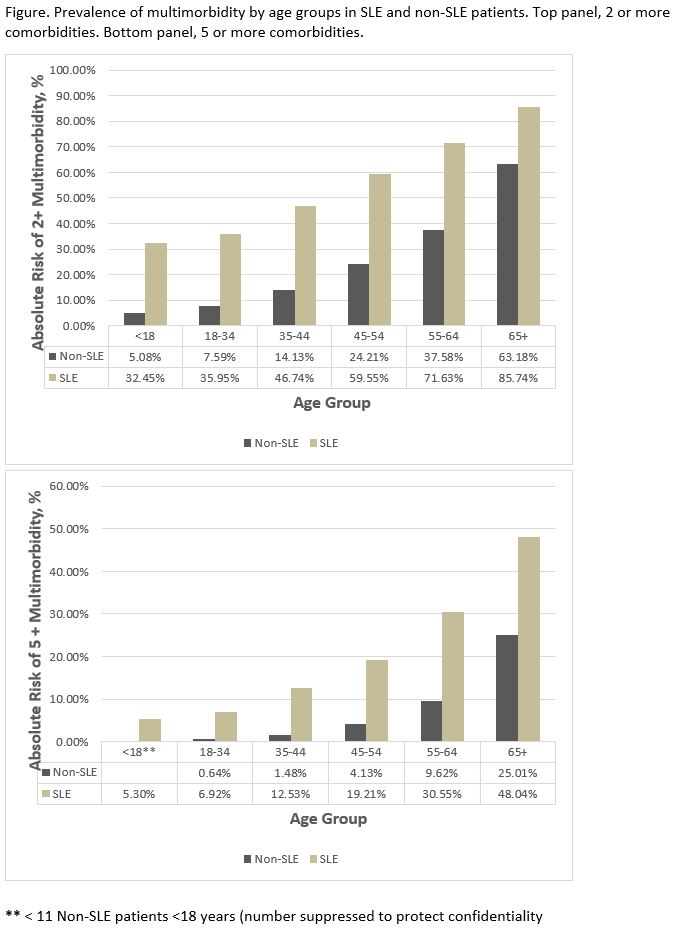
Results: 34,752 cases with SLE and 34,752 matched non-SLE comparators were included. Mean age was 48 (SD 14.2) years, and 90.6% were female for both cohorts. 66.4% of the patients in both cohorts were White, 18.4% Black, 3.4% Asian and 18.4% Hispanic. 1.3% of patients were < 18 years old; 17% 8-34; 21.3% 35-44; 27.1% 45-54; 22.1% 55-64 and 11.2% >65 years. Patients with SLE had more multimorbidity than non-SLE subjects (58.1% vs 26.3%). Multimorbidity increased with age in both cohorts (figure). Multimorbidity differences between SLE and non-SLE were present throughout all the age groups, in general patients with SLE compared to non-SLE had a difference of 27-34% in the prevalence of multimorbidity on all age groups except those age >65 where the difference was 23%. Young patients with SLE had a multimorbidity burden similar to non-SLE comparators who were three decades older (SLE 18-34, 35.95%, non-SLE 55-64, 37.58%). Young patients with SLE were 6-9 times as likely to suffer from multimorbidity compared to matched non-SLE patients in the same age group (table), these differences decreased in older age groups but persisted even in those SLE patients that were >65 (OR 3.5, 95%CI 3.12-3.90). Secondary analysis on patients with 5 or more comorbid conditions showed similar findings (figure and table).
Conclusion: This large nationwide study showed increased occurrence of multimorbidity in SLE versus non-SLE patients, with substantial burden of multimorbidity through all age groups and even persistent during elderhood. Young patients with lupus have a multimorbidity burden of similar to individuals 3 decades older. This study highlights the striking comorbidity burden patients with lupus endure. The effects of multimorbidity on compliance, healthcare burden and outcomes deserve further research.
To cite this abstract in AMA style:
Duarte-Garcia A, Heien H, Shah N, Crowson C. Multimorbidity Differences Between Systemic Lupus Erythematosus Patients and Comparators in Different Age Groups: A Large Nationwide US Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/multimorbidity-differences-between-systemic-lupus-erythematosus-patients-and-comparators-in-different-age-groups-a-large-nationwide-us-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multimorbidity-differences-between-systemic-lupus-erythematosus-patients-and-comparators-in-different-age-groups-a-large-nationwide-us-study/