Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: The syndrome of knee pain and meniscal tear (MT) is prevalent and disabling. The TeMPO trial (Treatment of Meniscal Problems in Osteoarthritis (OA)) compares the efficacy of in-clinic PT (true PT and sham) with a home exercise program in persons with symptomatic meniscal tear and OA.
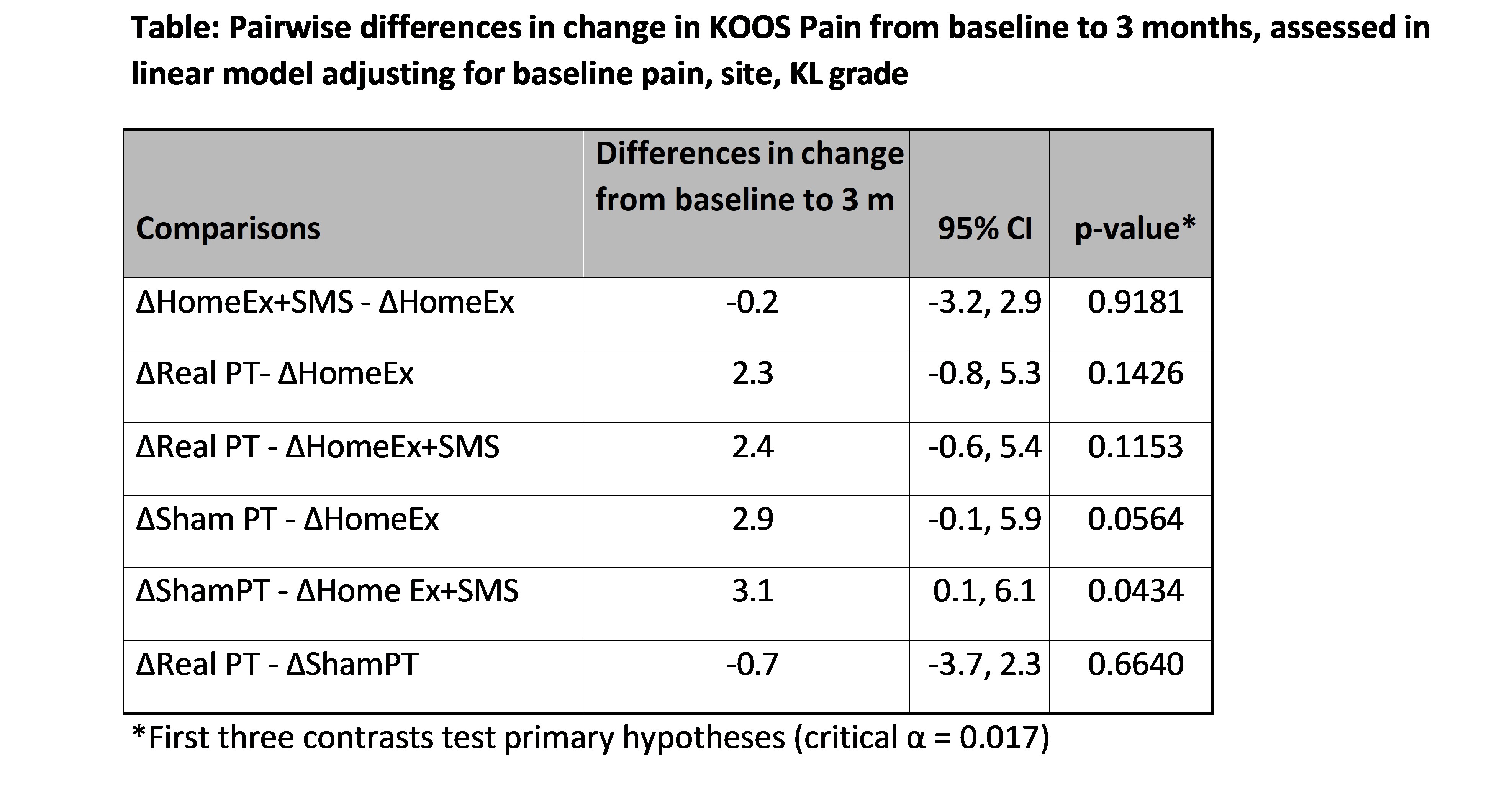
Methods: TeMPO is a 4-center RCT of 4 strategies: 1) Home exercises (HomeEx) focused on strengthening and stretching; 2) Home exercises + SMS messaging 3x per week to motivate adherence (HomeEx+SMS); 3) Home exercise, SMS, + PT focused on strengthening, manual therapy, and neuromuscular function (True PT)); and 4) Home exercise, SMS + sham PT consisting of ultrasound with energy turned off and light massage distant from the knee joint (Sham PT)). The sham and true PT regimens were delivered in 14 sessions over 12 weeks. The primary outcome was change in KOOS Pain between baseline and 3-months, assessed in a linear regression model adjusting for site, baseline Kellgren-Lawrence (KL) grade, and baseline KOOS Pain. A secondary outcome was treatment failure at 3 months, defined as failing to improve by 8 points in KOOS Pain, or receiving an intraarticular injection, or surgery. We assessed Pain Scores across baseline, 3, 6, and 12 months in a repeated measures model that adjusted for site and baseline KL.
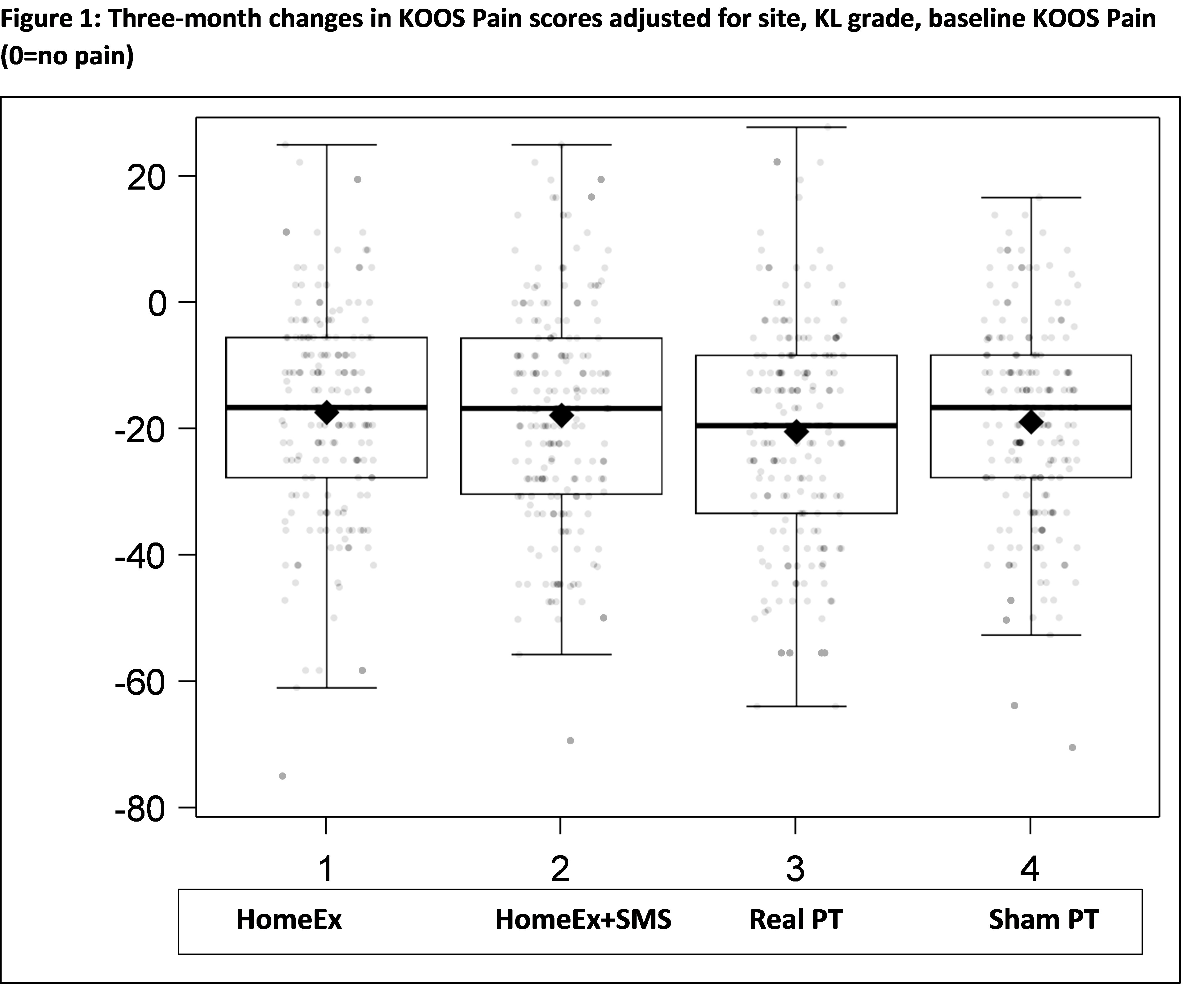
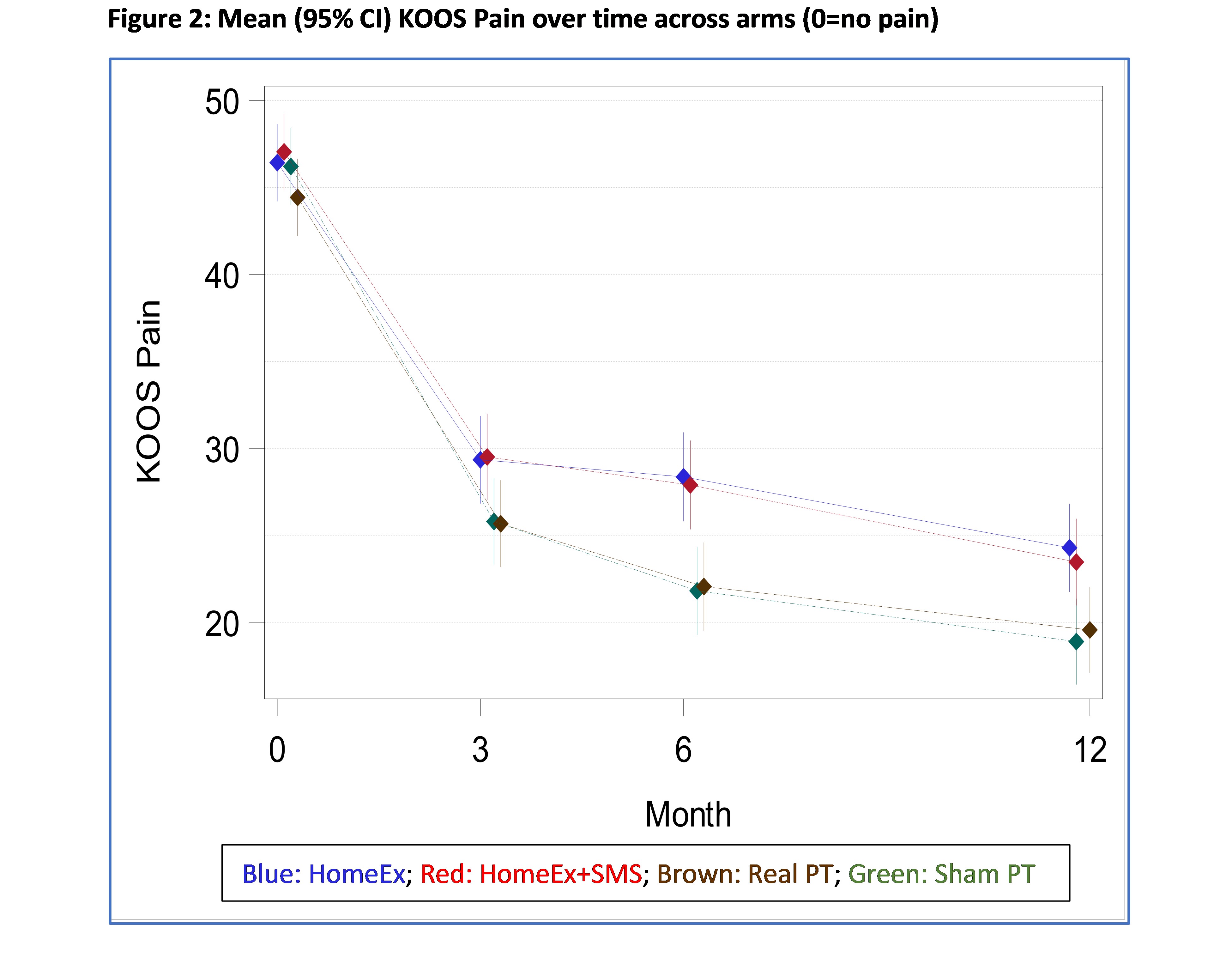
Results: At baseline the 879 randomized subjects had mean age 59.2 (SD 7.8), mean BMI 29.3 (SD 6.5), 57% female, and 33% KL 3. We obtained outcome data on 87% of subjects at 3 months and 83% at 12 months. Baseline KOOS Pain score (0-100 with 100 worst) was 46.1 (SD 15.5). The mean (SD) improvement in KOOS Pain at 3 months was 18.6 (SD 16.9) points in the whole cohort with no clinically important or statistically significant differences between any of the arms (Table1 and Figure 1). All subjects improved from baseline to 3 months by a mean of ~15% on strength in the quadriceps, hamstring, and gluteus medius muscles with no differences across groups. 30-36% of subjects experienced treatment failure (36% with HomeEx, 32% with HomeEx+SMS, 30% with Sham PT and 35% with True PT; p=0.58). The repeated measures analysis (Figure 2) showed that at 12 months the True PT and Sham PT groups reported greater improvement in pain (by ~5 KOOS points, 30% of a SD) than the groups that were not randomized to see a physical therapist, with no clinically important or statistically significant differences between the True PT and Sham PT groups.
Conclusion: At 3 months all treatment groups experienced clinically relevant improvement in pain and muscle strength with no clinically important or statistically significant differences in pain relief between any of the treatment arms. Electronic reminders to comply with the home exercise program did not provide discernable benefit. By12 months, subjects randomized to see a physical therapist reported greater improvement in pain scores (by 5 points) than those that did not see a therapist, with identical improvement in the sham PT and real PT groups. These findings point to delayed and sustained benefit from seeing a physical therapist and suggest the active ingredient in the PT program may have been interaction with the therapist rather than manual therapy or supervision of strengthening exercises.
To cite this abstract in AMA style:
Katz J, Collins J, Bisson L, Selzer F, Jones M, Yang H, Irrgang J, Safran-Norton C, Spindler K, Losina E. Multicenter Randomized Controlled Trial of Physical Therapy (PT) or Sham PT in Persons with Knee Pain, Meniscal Tear, and Osteoarthritic Imaging Changes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/multicenter-randomized-controlled-trial-of-physical-therapy-pt-or-sham-pt-in-persons-with-knee-pain-meniscal-tear-and-osteoarthritic-imaging-changes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multicenter-randomized-controlled-trial-of-physical-therapy-pt-or-sham-pt-in-persons-with-knee-pain-meniscal-tear-and-osteoarthritic-imaging-changes/