Session Information
Date: Sunday, November 17, 2024
Title: Abstracts: Innate Immunity: Molecular Insights Into Immune Dysregulation
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: The SITRAME syndrome (Systemic Inflammatory Trunk Recurrent Acute Macular Eruption) is a newly described inflammatory entity affecting adult patients with no family history (Soria et al 2022). Patients present with recurrent flares of truncal rash (Fig 1.) associated with fever, asthenia and biological inflammation, most commonly following a history of viral infection or mRNA vaccination. In this study, we aim to identify the inflammatory pathway(s) involved in the disease.
Methods: 14 patients were recruited to perform a multi-level characterisation of the disease using blood samples. This characterisation includes cellular phenotyping by flow cytometry, assessment of plasmatic cytokine levels by ELISA, assessment of cellular cytokine production by flow cytometry and transcriptomic analysis by RNA-sequencing. For each data, results from healthy donors, patients in the basal state and patients in the flare state were evaluated.
Results: Patients all had SITRAME defined criteria (Soria et al, 2024). The sex ratio of patients was 1:1 and the median age of onset was 29 years, ranging from 18 to 45 years. 92.8% of patients (13/14) presented with flares following a history of viral infection or mRNA vaccination, compared with 73.3% (22/30) of all known SITRAME patients. The median CRP level during a flare was 22mg/L, ranging from 8 to 100mg/L.
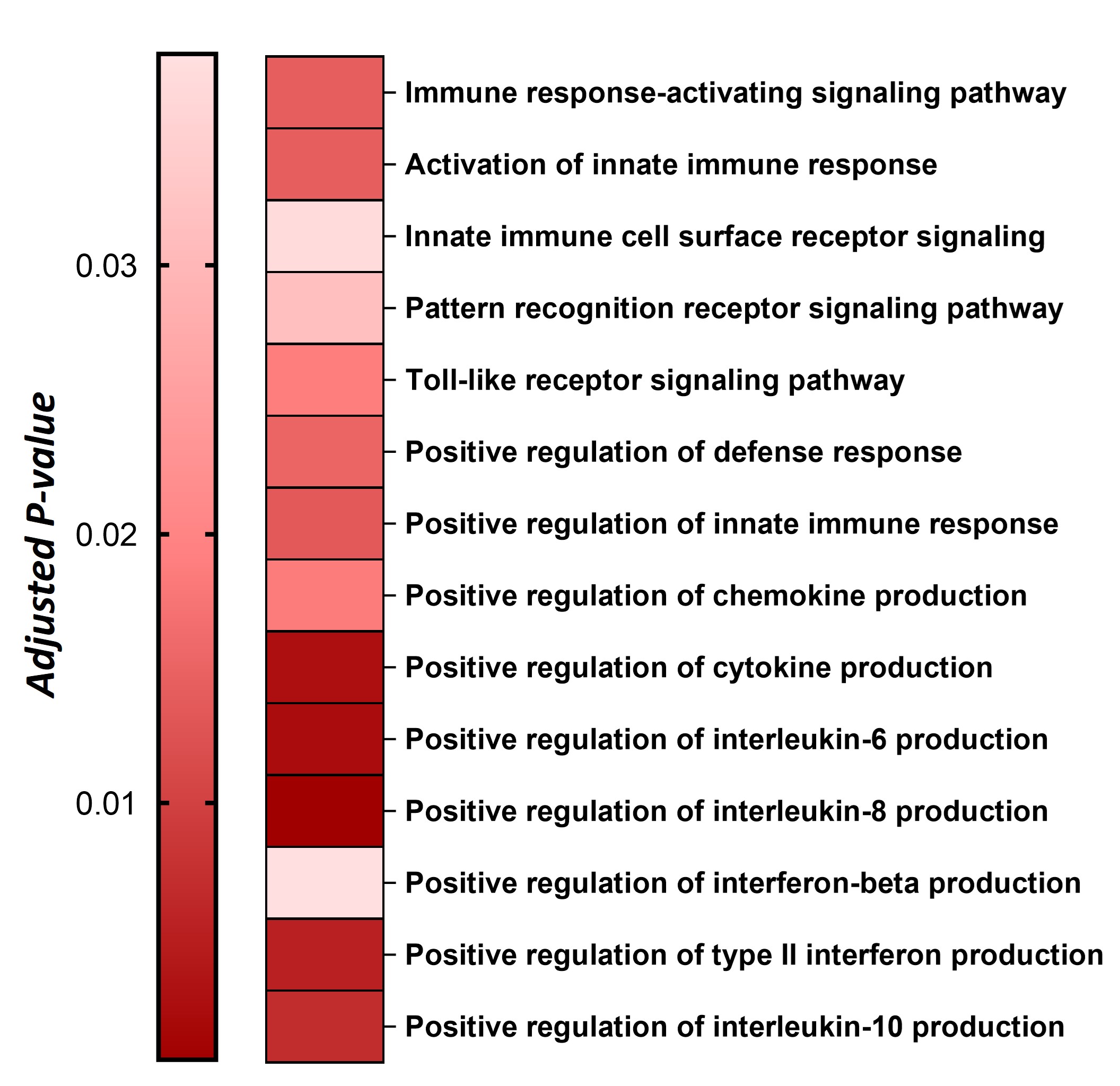
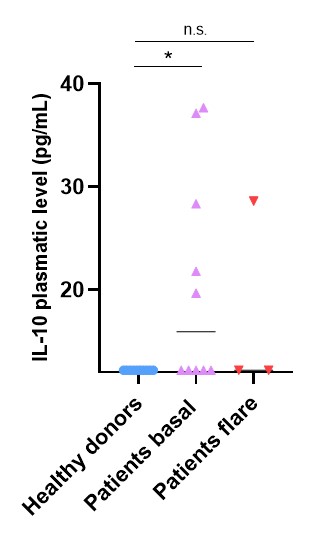
In the basal state, patients share a common transcriptomic signature consisting of innate immune cell activation. They also show activation of the anti-inflammatory IL-10 production pathway at the transcriptomic level (Fig 2.), which correlates with higher levels of plasmatic IL-10 compared to healthy donors (Fig 3.).
In the flare state, they specifically show a transcriptomic type I interferon signature and higher plasmatic levels of IFNα and CXCL10. Consistently, unstimulated monocytes and plasmacytoid dendritic cells from active patients produce IFNα. Flare state patients did not show the high levels of plasmatic IL-10 found in basal state patients (Fig 3.).
Conclusion: The SITRAME syndrome is an adult onset disease characterised by an innate immune inflammatory background and dysregulation of the type I interferon pathway during flares. The results also support immune regulation by IL-10 in the basal state, which is lost when patients are in flare state. Further ongoing analysis should help to determine the relative genetic and environmental contributions to this disease.
To cite this abstract in AMA style:
Zhu Y, Soria A, Moreau T, Boursier G, Bondet V, Donnadieu F, Cretet C, Haddouche A, Schmidt C, Bletry D, Amsler E, Barbaud A, Rahal F, Chantran Y, Cescato M, Maillet F, Korganow A, Chaigne B, Dieudonné Y, Lefevre G, Miyara M, Beziat V, Deswarte C, White M, Georgin-lavialle S, duffy D, Rodero M. Multi-omic Study in Patients with SITRAME Syndrome [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/multi-omic-study-in-patients-with-sitrame-syndrome/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multi-omic-study-in-patients-with-sitrame-syndrome/