Session Information
Date: Saturday, November 12, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: There is growing evidence revealing that females report worse patient-reported outcomes compared to males in axial spondyloarthritis (axSpA). However, in which precise outcomes there is a meaningful difference across gender and whether this also occurs in patients with peripheral spondyloarthritis (pSpA) and psoriatic arthritis (PsA) is not fully understood. The aim of this study was to investigate the influence of gender on disease outcomes in patients with SpA, including axSpA, pSpA and PsA, in a worldwide setting.
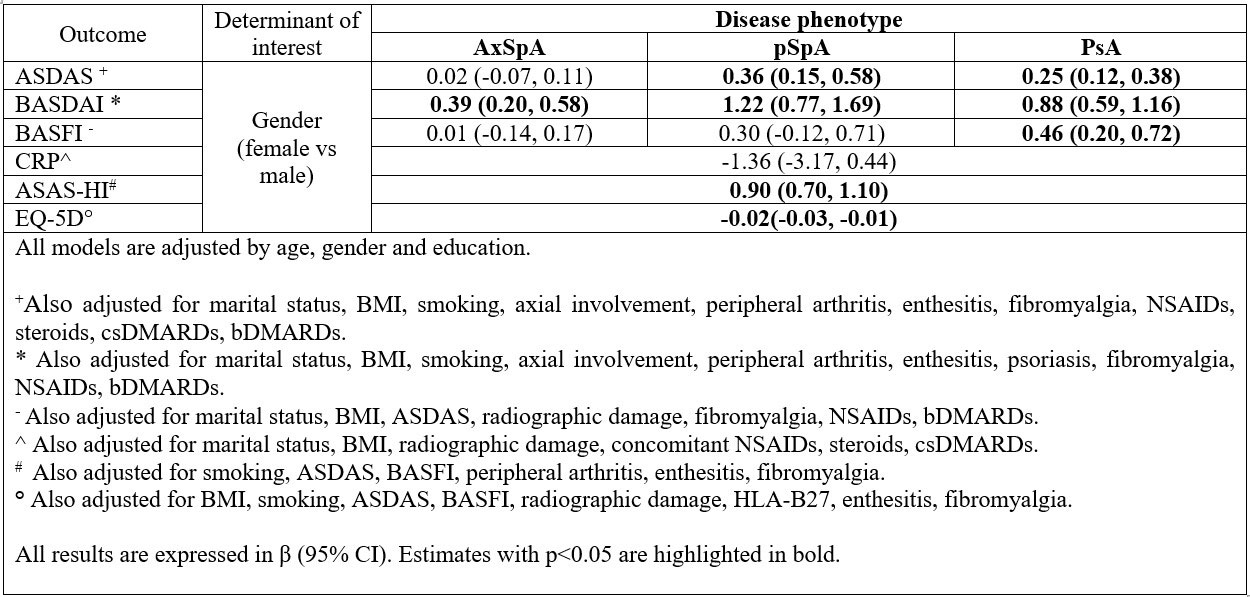
Methods: Data from 4185 patients with axSpA, pSpA or PsA from the ASAS-PerSpA study were analysed. The ASAS-PerSpA is a cross-sectional study that recruited consecutive patients with SpA (according to their rheumatologist) from 24 countries. Associations between gender and disease activity [Ankylosing Spondylitis Disease Activity Score (ASDAS), Bath Ankylosing Spondylitis Disease Activity Score (BASDAI), C-reactive protein (CRP)], function [Bath Ankylosing Spondylitis Functional Index (BASFI)], and overall health [ASAS-Health Index (ASAS HI), European Quality of Life Five Dimension (EQ-5D)] were investigated. Multilevel (country) univariable and multivariable linear mixed models were used. Interactions between gender and disease phenotype (SpA, pSpA and PsA) were analysed, and if relevant, models were stratified by disease subtype. Models were adjusted for relevant confounders (Table).
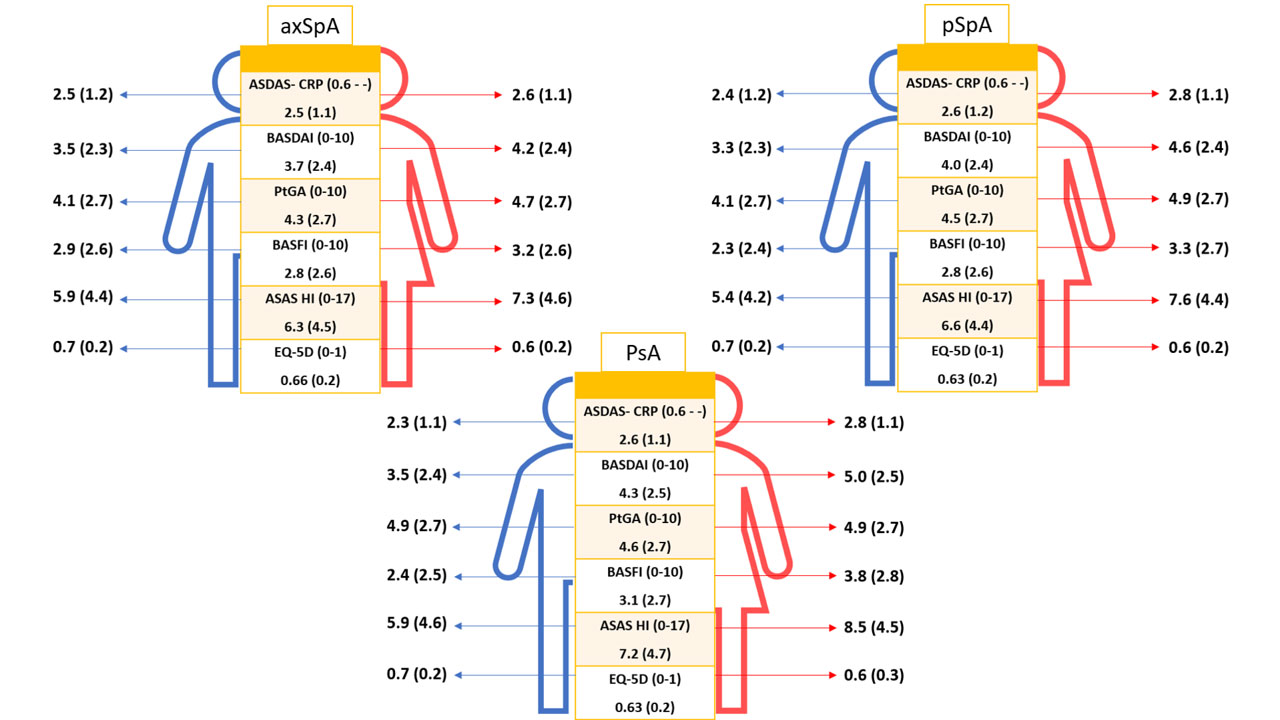
Results: In total, 4185 patients were included, of which 2719, 1033 and 433 had a diagnosis of axSpA (mean age 42 years, 32% female), PsA (mean age 52 years, 52% female) and pSpA (mean age 44 years, 53% female), respectively. Female patients consistently reported worse outcomes than males across the SpA spectrum in terms of disease activity, functional disability, and overall health (Figure). A significant interaction between gender and disease phenotype was found for ASDAS, BASDAI and BASFI. Multivariable models for each outcome are shown in Table (stratified by disease phenotype). While being female independently contributed to higher BASDAI across the three disease phenotypes (though with varying magnitude), female gender was only associated with higher ASDAS in pSpA [β (95% CI): 0.36 (0.15, 0.58)] and PsA [0.25 (0.12, 0.38)] but not in axSpA [0.016 (-0.07, 0.11)]. Female gender was associated with higher BASFI in PsA [0.46 (0.20, 0.72)]. No associations were observed between gender and CRP levels. Female gender was associated with higher ASAS-HI [0.90 (0.70, 1.10)] and EQ5D [-0.02 (-0.03, -0.01)], without significant differences across disease phenotype.
Conclusion: Female gender was associated with less favorable outcomes across the SpA spectrum, except for CRP in which there were no differences between gender. While female gender influenced BASDAI across disease phenotypes, ASDAS was not associated with gender in axSpA. These results suggests that ASDAS should be the preferred instrument in clinical practice both for females and males with axSpA.
To cite this abstract in AMA style:
Benavent D, Capelusnik D, Ramiro S, Molto A, Lopez-Medina C, Dougados M, Navarro-Compán V. Most Disease Outcome Measures but Not ASDAS Are Influenced by Gender in Patients with Axial SpA: Results from ASAS-PerSpA [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/most-disease-outcome-measures-but-not-asdas-are-influenced-by-gender-in-patients-with-axial-spa-results-from-asas-perspa/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/most-disease-outcome-measures-but-not-asdas-are-influenced-by-gender-in-patients-with-axial-spa-results-from-asas-perspa/