Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Achieving health equity has been a long-standing goal, as Academy of Medicine leaders stated, ‘There is no equity without quality, and there is no quality without equity.” In its 5-year strategic plan, the ACR Quality Measures Subcommittee (QMS) requested 4 working papers at the intersection of quality measurement; herein we address health equity through measurement. We convened diverse collaborators aiming to: 1) summarize existing health disparities in the ACR’s RISE registry defining known and unknown health equity issues in rheumatology; 2) envision an ideal future state; and 3) create a roadmap for how the ACR can advance health equity in rheumatology through quality measurement.
Methods: The workgroup consisted of 20 ACR members, including members of QMS, Diversity, Equity & Inclusion (DEI), and Registries and Health IT committees, a patient representative and an ARP member. Members represented academics, private practice, racial, ethnic, and geographic diversity. The workgroup met virtually monthly in 2023, and twice in 2024. We used the CMS and National Institutes of Health PROGRESS PLUS acronym to frame groups at risk for disparities. Members reviewed the existing 25 ACR quality measures, and used modified Delphi panel voting on items’ impacts on health equity and quality (0-10 scale).
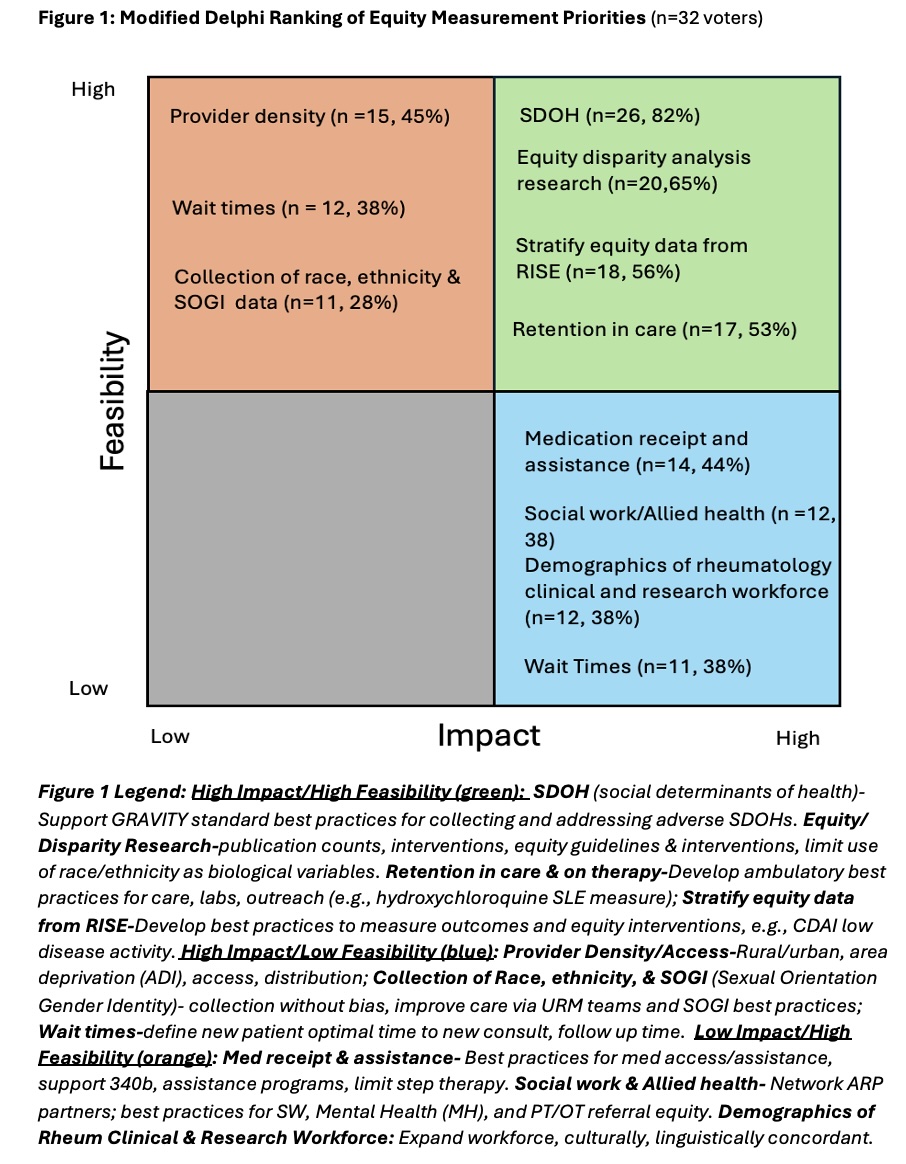
Members next envisioned ideal state components and equity steps that ACR and rheumatology could achieve. Ideas were ranked 0-10 for feasibility and impact, then grouped per NCQA’s Health Measurement Framework for Medicaid Accountability Equitable Social Interventions, adding an Equitable Research domain. We prioritized recommendations using nominal group technique, ranking first internally, and then with input from the ACR QMS and DEI and Collaborative Initiatives (COIN) Committees.
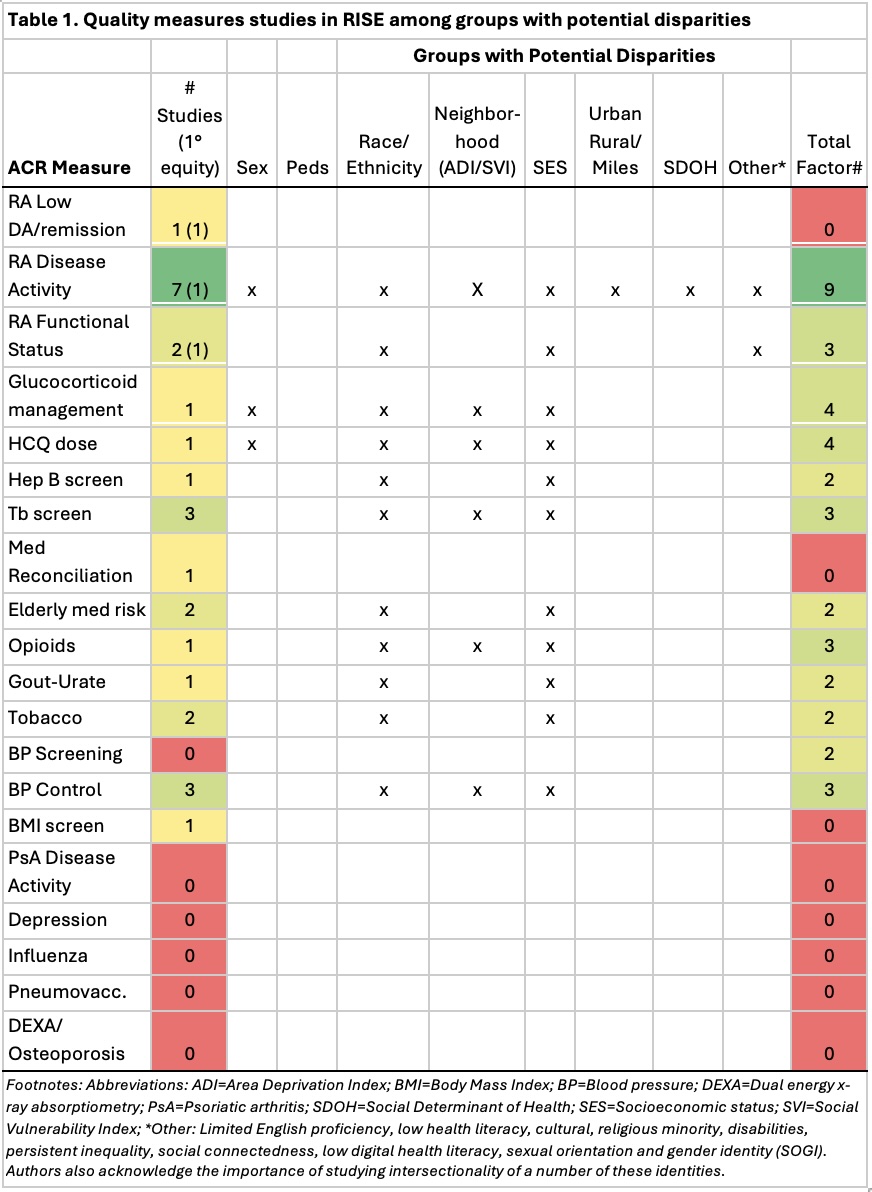
Results: Among 25 existing measures, only 3 had RISE studies focused on disparities as the main explanatory variable (Table 1). Few studies examined quality performance stratified by demographic factors to assess for variation in outcomes. Rheumatoid arthritis disease activity was most heavily studied, with 7 studies evaluating equity domains, though only 1 as a primary covariate.
Results of prioritizing are shown in Figure 1 (n= 32 raters). Highest ratings for feasibility and impact supported screening and referral best practices for SDOHs and supporting GRAVITY standards (26, 82%), equity and disparities research best practices (20, 63%), stratifying data for equity outcomes in RISE (for ACR quality measures (18, 56%) and developing practices to support retention in care (17, 53%). Defining standards for wait times for new and return patients had many split votes for high feasibility/low impact, (11, 34%) and low feasibility/high impact (12, 38%). Items rated as low feasibility/high impact included: medication receipt/assistance (14, 44%), social work/allied health (12, 38%), and team demographics matching patient populations (12, 38%).
Conclusion: The working group identified gaps at the intersection of equity and quality and opportunities within the RISE registry. Recommendations for advancing equity through quality measurement were generated to inform developing a roadmap for the ACR to advance quality and equity.
To cite this abstract in AMA style:
Ferguson S, Anandarajah A, Wells M, Bekele D, Blazer A, Crowson C, Desir D, Ferucci E, Machua W, Morgan E, Rogers W, Smith L, Zell J, Suter L, Jatwani S, Bartels C. Modified Delphi Process to Propose an Equity Measurement Roadmap in Rheumatology [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/modified-delphi-process-to-propose-an-equity-measurement-roadmap-in-rheumatology/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/modified-delphi-process-to-propose-an-equity-measurement-roadmap-in-rheumatology/