Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: For most patients with diffuse cutaneous systemic sclerosis (dcSSc), skin thickness improves over time, especially with background immunosuppressive treatment. This has reduced confidence in group level skin score (mRss) change as a meaningful endpoint in clinical trials that may not convincingly demonstrate greater improvement in active treatment arms compared to control. Nevertheless, skin thickening contributes significantly to dcSSc morbidity. We explore the association between skin change over time and outcomes in a cohort of early dcSSc patients.
Methods: DcSSc subjects with at least one mRss assessment within the first 5 years from onset were included. Observed change in mRss between first assessment and 12(±2) months follow-up was calculated and categorised as improvement, if there was a decline by ≥ 5 units or 25%; worsening, if we observed increase by ≥ 5 units or 25% and stable, if change was within 5 units and 25%. Random effect models were fitted to evaluate continuous changes in mRss over time. Model-predicted individual patient intercept and slope were used to assess association between absolute mRss at baseline (12 months from onset), mRss change and time to death or development of organ disease.
Results: Of the 467 patients, 106 (22.7%) were male and mean age of disease onset was 45.5 (SD 13.2) years. Most frequent autoantibodies were anti-topoisomerase I antibody (ATA) in 141 (30.2%) and anti-RNA polymerase antibodies (ARA) in 140 (30.0%) of the subjects. Other antibodies included anti-U3RNP in 32 (6.9%), anti-PmScl in 21 (4.5%) and 73 (15.6%) of the subjects were ANA positive, but ENA negative (ANA+ENA-). In 94 patients (20.1%) mRss was assessed once, while 278 (59.5%) had three or more mRss assessments.
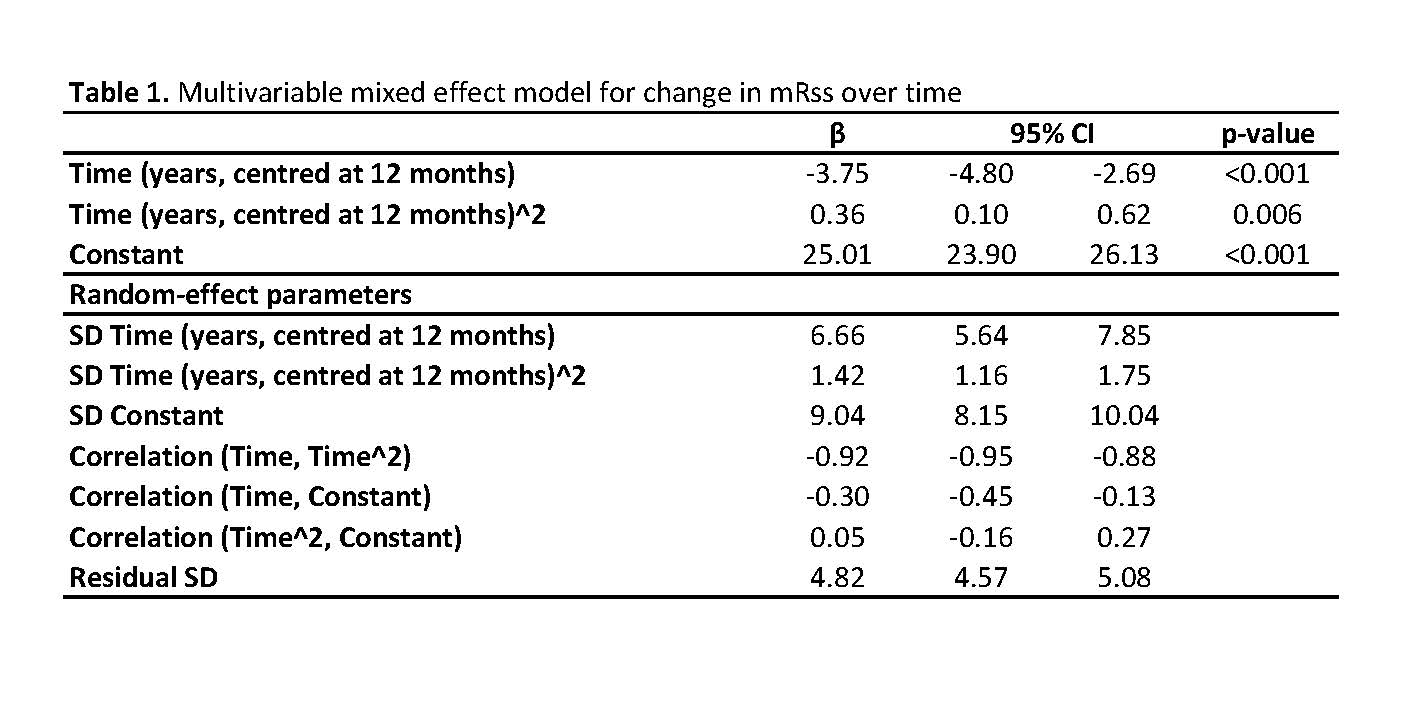
Average mRss at 12 months from onset was estimated to be 25 and there was consistent decline over subsequent years, which slowed down with longer disease duration (3.4, 2.7, 1.9 and 1.2 units at years 2, 3, 4 and 5). As previously shown, there was a weak negative correlation between mRss at 12 months and subsequent change (correlation coefficient -0.3), suggesting higher initial mRss associates with greater subsequent decline (Table 1).
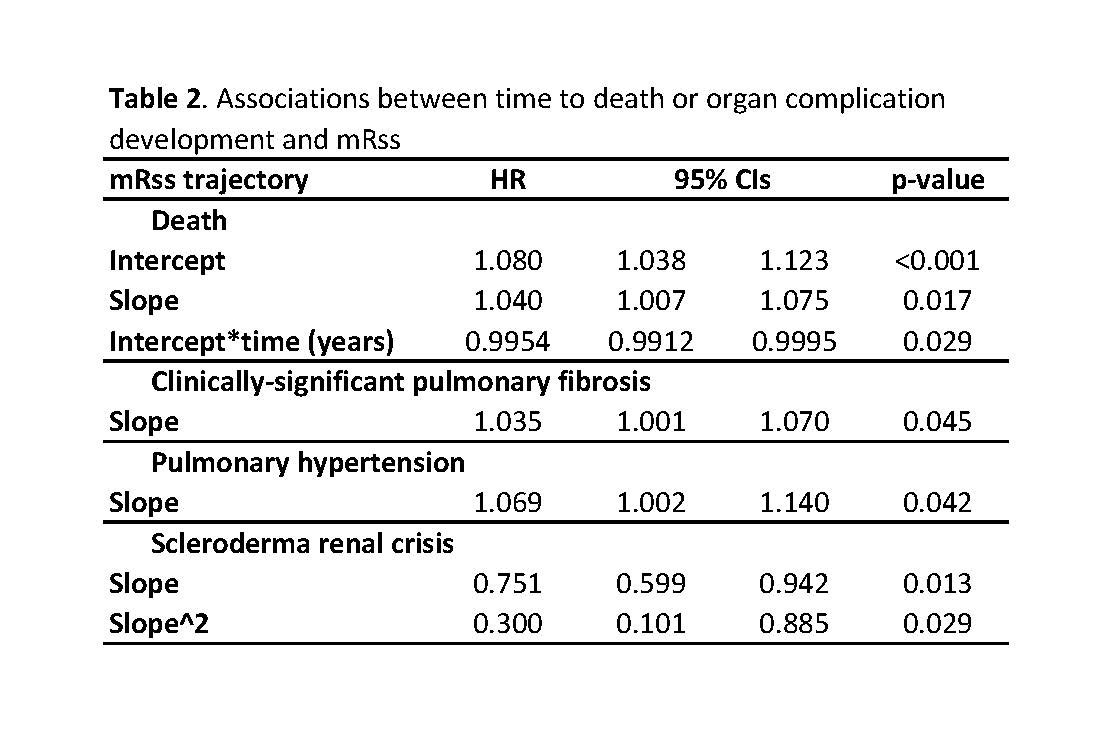
Of the 147 patients who had two mRss assessments within 12(±2) months, only 12.9% had worsening mRss, 34.7% had improvement and the majority (52.4%) experienced very little change. Both higher intercept and higher slope predicted increased risk of death with 8% increase in hazard for every unit higher baseline mRss and 4% increase for every unit higher change per year (Table 2). Pulmonary fibrosis and pulmonary hypertension development associated with higher change in mRss, but not with baseline absolute mRss values (3.5% and 7% increase in the hazard respectively for one unit higher mRss change over 12 months). It appeared that higher slope associated with lower hazard of scleroderma renal crisis, while we found no associations between skin and cardiac SSc.
Conclusion: Skin changes over the initial 5 years of disease vary between patients. At a group level there is an improvement, however, for individual patients slower improvement or deterioration in skin predicts increased risk of pulmonary complications and higher mortality rates.
To cite this abstract in AMA style:
Nihtyanova S, Derrett-Smith E, Fonseca C, Ong V, Denton C. Modelled Patient Level Skin Score Trajectory Predicts Risk of Death or Major Organ-Based Complications in Diffuse Cutaneous Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/modelled-patient-level-skin-score-trajectory-predicts-risk-of-death-or-major-organ-based-complications-in-diffuse-cutaneous-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/modelled-patient-level-skin-score-trajectory-predicts-risk-of-death-or-major-organ-based-complications-in-diffuse-cutaneous-systemic-sclerosis/