Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Adverse drug events (ADEs; harm from use of a drug) cause a significant burden to the healthcare system, with an estimated 5% of hospitalizations being drug-related. Up to 80% of ADEs may be preventable; and up to 20% of medication-related events may be related to non-adherence or drug omissions (including non-use of an indicated medication, i.e. prophylactic therapies). People with systemic lupus erythematosus (SLE) take multiple medications, increasing risk of ADEs and other medication-related adverse events. Within the McGill University Health Centre (MUHC) SLE cohort, we estimated the frequency and preventability of hospitalizations related to ADEs and medical omissions.
Methods: All patients in the SLE cohort satisfy the 1997 American College of Rheumatology (ACR) classification criteria and were enrolled after diagnosis. We identified consecutive MUHC admissions among SLE cohort participants between 2015-2020. For each hospitalization, we recorded home medications, admission diagnosis, and outcomes of ADEs and drug omissions. Two adjudicators independently evaluated each hospitalization using the Leape and Bates method, to rank confidence that an ADE or drug omission contributed to the admission (1=little/no confidence; 6=virtually certain). We computed a kappa statistic to assess inter-rater reliability. A third adjudicator helped resolve 7 unclear cases. Medication-related events were then classified as potentially preventable or ameliorable, or not, and potentially modifiable factors were identified.
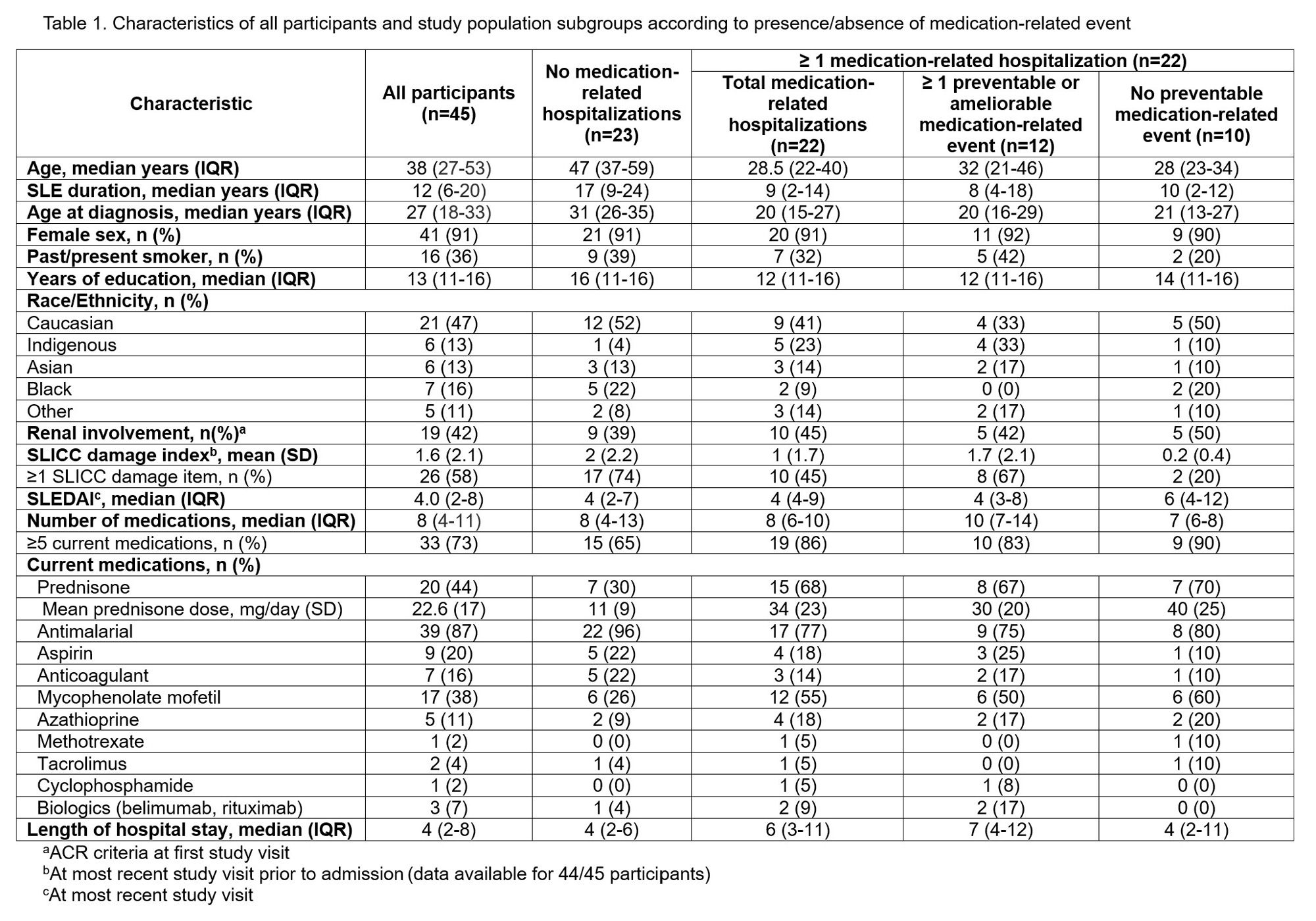
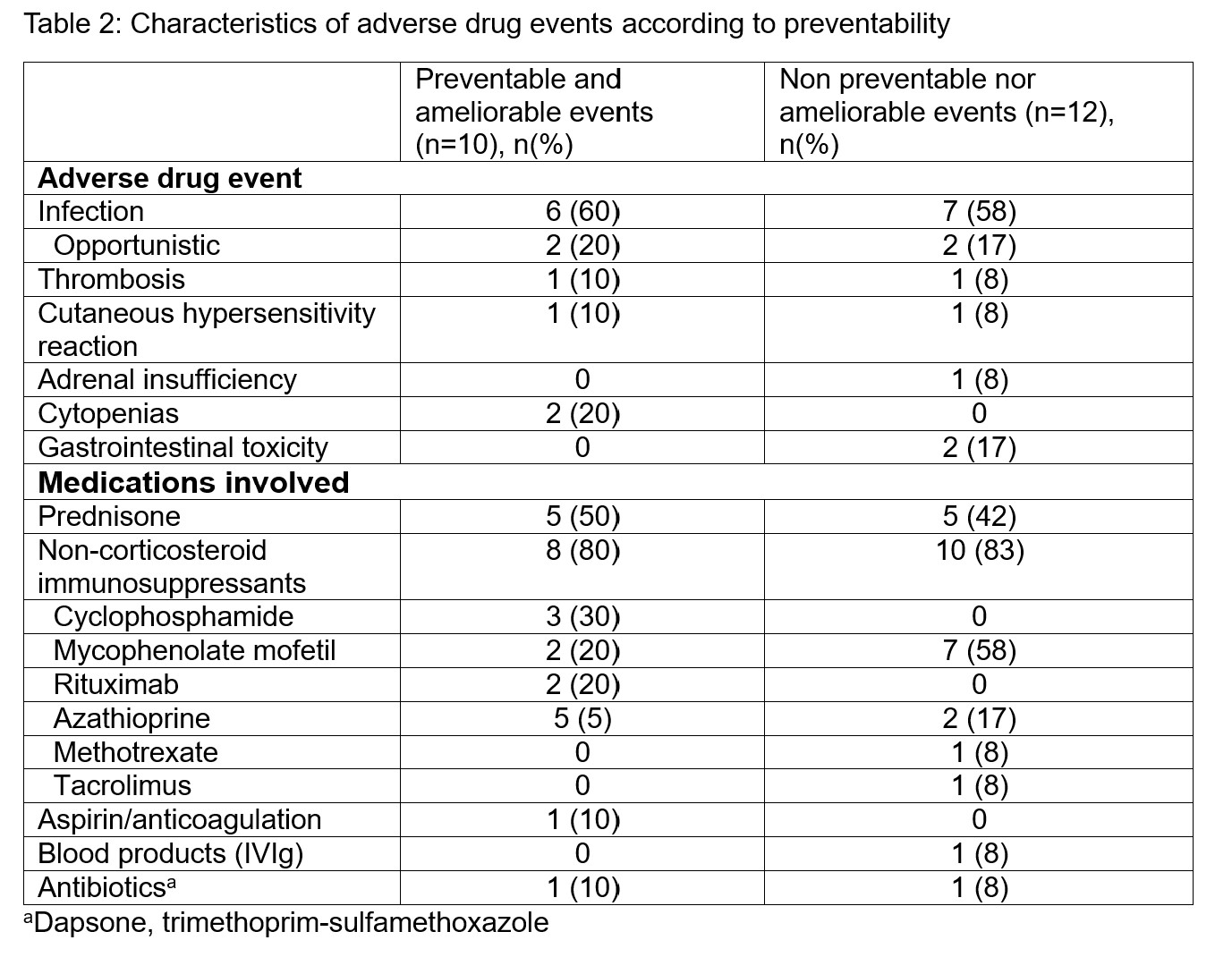
Results: Among 481 SLE cohort members followed between 2015-2020 (2303 person-years), 67 hospitalizations occurred (3 hospitalizations/100 person-years) among 45 participants. At first admission, median age was 38 years (interquartile range, IQR 27-53), median disease duration was 12 years (IQR 6-20), and participants’ home medications numbered a median of 8 (IQR 4-11). Forty one (91%) were female, and >50% were non-Caucasian. Over a quarter (n=19, 28%) of hospitalizations were likely due to one or more ADE (Leape and Bates scores 4-6). Initial unweighted kappa for adjudication was 0.7. ADEs (n=22) included infections (n=13, 59%), cutaneous hypersensitivity reactions (n=2, 9%), adrenal insufficiency (n=1, 5%), drug toxicity (n=4, 18%), and thrombosis (n=2, 9%). Prednisone (n=10, 45%) and/or other immunosuppressants (n=18, 82%) were commonly involved. Eight (12%) hospitalizations related to drug omissions, of which 7 (10%) were flares due to non-adherence. Excluding these flares, 11 medication-related events (48%) were potentially preventable/ameliorable. Modifiable factors included timely glucocorticoid tapering (n=3, 25%), promptly acting on laboratory results (n=4, 33%), and preventative strategies (thromboprophylaxis, vaccination, infection screening; n=3, 25%).
Conclusion: In our SLE cohort, 40% of hospitalizations were medication-related, most often due to ADEs. At least half of medication-related hospitalizations were potentially preventable or ameliorable. Infection prevention should be a priority in this group.
To cite this abstract in AMA style:
Stanciu M, Vinet E, McDonald E, Clark G, Pineau C, Kalache F, Grenier L, Bernatsky S, Mendel A. Medication-related Hospitalizations in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/medication-related-hospitalizations-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/medication-related-hospitalizations-in-systemic-lupus-erythematosus/