Session Information
Date: Tuesday, November 14, 2023
Title: (2039–2060) Pediatric Rheumatology – Clinical Poster III: Potpourri
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: This study aims to determine the prevalence of medical trauma and its impacts on outcomes in a sample of children with inflammatory arthritis. We hypothesize that medical trauma is an underrecognized entity in this population, and that it is associated with worse pain outcomes and disability risk.
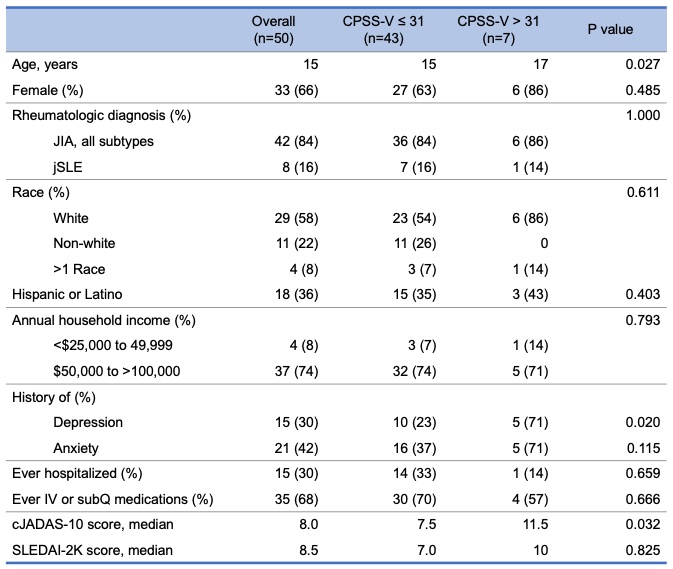
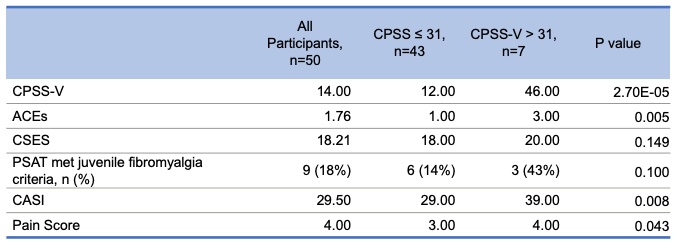
Methods: Children aged 8-18 years with juvenile idiopathic arthritis (JIA) or juvenile lupus erythematosus (jSLE) with a history of inflammatory arthritis were recruited from a single center pediatric rheumatology clinic. Participants completed a questionnaire assessing for medical trauma related to their arthritis with an adapted Child PTSD Symptom Scale for DSM-V (CPSS-V). Further questionnaires assessed for self-efficacy to function despite pain (Child Self-Efficacy Scale), pain scores (Verbal Rating Scale, 0-10), juvenile fibromyalgia (JFM) (Pain and Symptom Assessment Tool), anxiety sensitivity (Childhood Anxiety Sensitivity Index), and other adverse childhood experiences (ACEs). Demographic and disease activity data were collected. Differences between those with and without probable medical PTSD (CPSS-V score >31 vs ≤ 31) were assessed using rank sum and exact tests. Linear regression examined continuous associations with CPSS-V.
Results: Fifty children and adolescents with JIA (n=42) or jSLE (n=8) completed the study. Twenty (40%) children had CPSS-V scores of moderate or greater severity and 7 (14%) scored in the probable medical PTSD range. Those with juvenile spondyloarthropathy and rheumatoid factor positive polyarticular JIA had the highest trauma scores, but there was no overall difference in trauma scores between JIA and jSLE. CPSS-V scores in the probable medical PTSD range were significantly associated with older age, higher pain and anxiety sensitivity scores, more ACEs and depression history, and higher JIA disease activity scores (cJADAS-10) but not jSLE activity scores (SLEDAI-2K). There was a trend towards poorer self-efficacy scores and meeting JFM criteria in the probable medical PTSD group. Poorer self-efficacy scores were significantly associated with higher CPSS-V scores when assessed as a continuous variable. Nine (18%) participants met criteria for JFM and had higher average trauma scores compared to those who did not. Trauma scores were not associated with history of hospitalization or injected medication use.
Conclusion: Medical trauma symptoms were reported by many participants in this cohort of children with inflammatory arthritis. Those who have experienced more trauma from their rheumatologic disease may be at risk for worse pain outcomes and increased disability, specifically poor self-efficacy and high anxiety sensitivity. Further studies are necessary to determine the true prevalence of medical trauma in this population, its impact on pain and disability, potential interventions, and the importance of trauma-informed care.
To cite this abstract in AMA style:
Medrano L, Bursch B, Weiss J, Hoftman A, Li J, Jackson N, McCurdy D. Medical Trauma and Its Association with Pain and Disability Risk in Children with Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/medical-trauma-and-its-association-with-pain-and-disability-risk-in-children-with-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/medical-trauma-and-its-association-with-pain-and-disability-risk-in-children-with-inflammatory-arthritis/