Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Non-infectious pediatric uveitis is a vision threatening disease whose treatment involves both ophthalmologists and rheumatologists.In other diseases necessitating multidisciplinary care, coordinated care clinics have shown improved outcomes.While many pediatric uveitis guidelines suggest that coordinated uveitis care is important, there is sparse data on its effectiveness.The objective of this study was to evaluate the impact of an Ophthalmology and Rheumatology Coordinated Care clinic on patients with anterior uveitis by comparing outcomes between those who received traditional care vs. coordinated care.
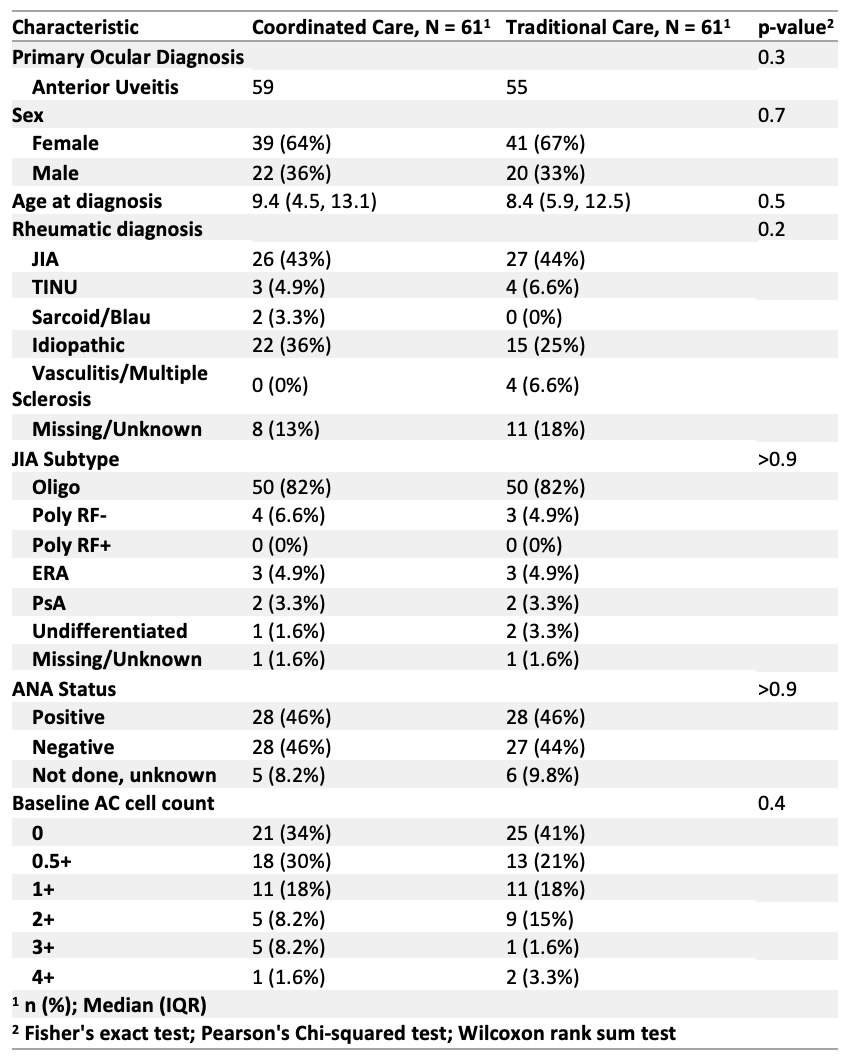
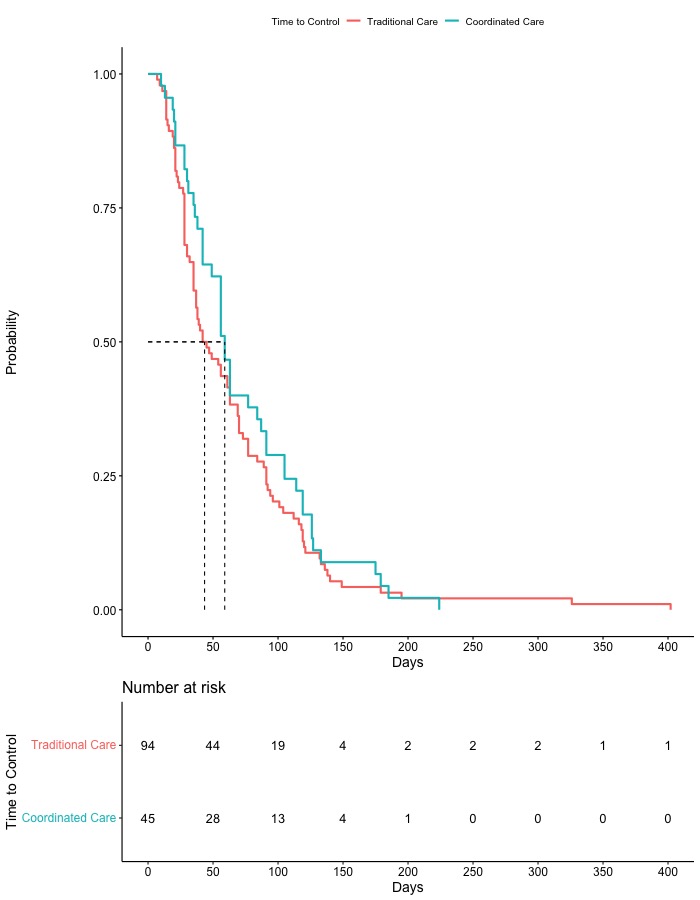
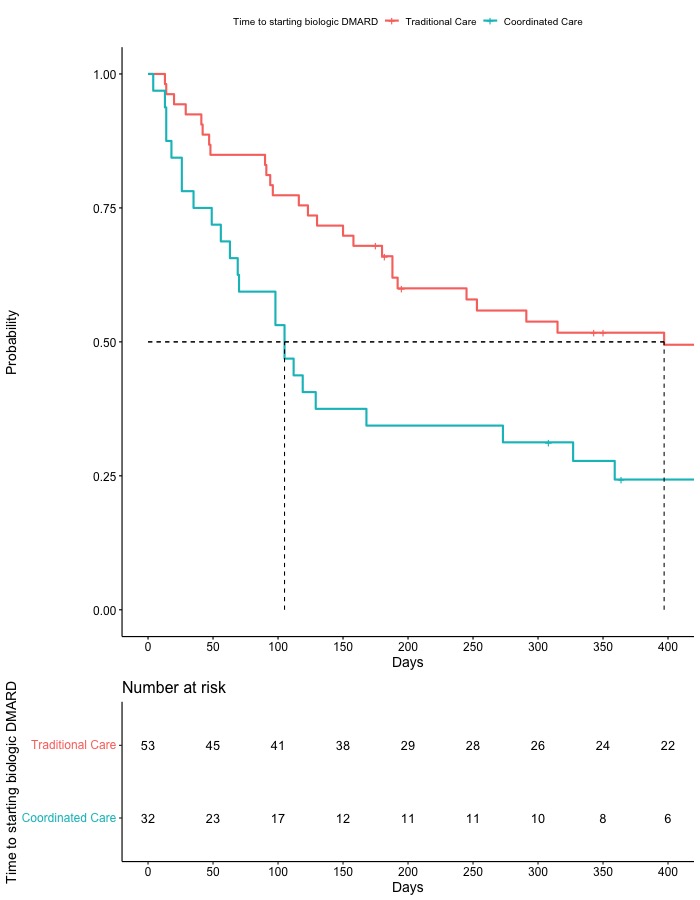
Methods: This was a retrospective cohort study of children ages ≤ 19 years, with anterior uveitis (AU) included in a registry from pediatric tertiary care center between 2013-2022. Inclusion criteria for the Uveitis Coordinated Care Clinic (coordinated care) cohort: ≥2 visits within the first 6 months of first coordinated care visit with ≥1 additional visit in the subsequent 6 months (minimum of 3 clinic visits within year 1). If criteria were not met, patients were assigned to the non-UCCC (traditional care) cohort. Start time into the coordinated care cohort was the first coordinated care visit in the registry and for the traditional care cohort was the first ophthalmology appointment in the registry. The patient could transition from traditional to coordinated care cohort and time in each could be counted for the disease control analysis. Disease control was defined as ≤0.5+ anterior chamber (AC) cell (as per SUN criteria) and ≤2 topical steroid drops daily. Standard descriptive statistics were used to describe clinical features including sex, age at diagnosis, and primary rheumatic diagnosis. Survival analysis was used to identify differences in cohort disease activity and biologic DMARDs use over time. Chi-square test of independence was used to examine differences in topical steroid use between cohorts at their initial visit and at 6 months.
Results: A total of 122 patients met inclusion criteria. Sixty-one in the coordinated care cohort and 61 in the traditional care cohort. There was no statistical difference between cohorts in the speed at which they achieved disease control (median time 44 (traditional care) vs 59 days (coordinated care), p = 0.3) (Figure 1). No patient level covariates such as baseline AC cell or duration of disease before cohort entry statistically impacted the outcome. The coordinated care cohort did start biologic DMARDs faster from entry into cohort than the traditional care cohort (p = 0.016) (Figure 2). The coordinated care cohort was on fewer steroid drops at baseline than the traditional care cohort. There was no difference in topical steroids at six months between cohorts.
Conclusion: In our current cohort, we did not demonstrate improved speed at which they achieved disease control, although they did initiate care sooner with biologics. Further analyses are needed to explore differences between the two cohorts such as number of recurrent disease activity, flares, and how potential confounding factors, such as entry time into each cohort might impact these results.
To cite this abstract in AMA style:
Lavallee C, Gmuca S, Lerman M. Measurable Outcomes of an Ophthalmology and Rheumatology Coordinated Care Clinic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/measurable-outcomes-of-an-ophthalmology-and-rheumatology-coordinated-care-clinic/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/measurable-outcomes-of-an-ophthalmology-and-rheumatology-coordinated-care-clinic/