Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Lower socioeconomic status is associated with greater disease activity and mortality in systemic lupus erythematosus (SLE); however, mechanisms driving this are yet to be understood. Qualitative research suggests that material need insecurities, such as concerns about housing, food, or medical costs, impair patients’ ability to manage SLE, exacerbating the effects of poverty. We describe the prevalence of food, housing, SLE healthcare, and financial insecurity in an SLE cohort and test their associations with patient-reported outcomes (PROs).
Methods: Data were derived from a statewide SLE epidemiology study involving a cohort of individuals with physician-confirmed SLE. Food, housing, healthcare, and financial material need insecurities were assessed by validated screening tools. PROs were obtained via PROMIS, Neuro-QoL, Patient Health Questionnaire-8, and General AnxietyDisorder-7 instruments. Poverty was defined as household income ≤125% of the federal poverty limit.Lower education was defined as less than a bachelor’s degree. The association of material need insecurities with PROs was assessed by multivariable linear regression models adjusting for demographics, lupus characteristics, and comorbidities. We examined the relationship between insecurities with poverty and education via unadjusted ANOVA and by including interaction terms in the adjusted regression model.
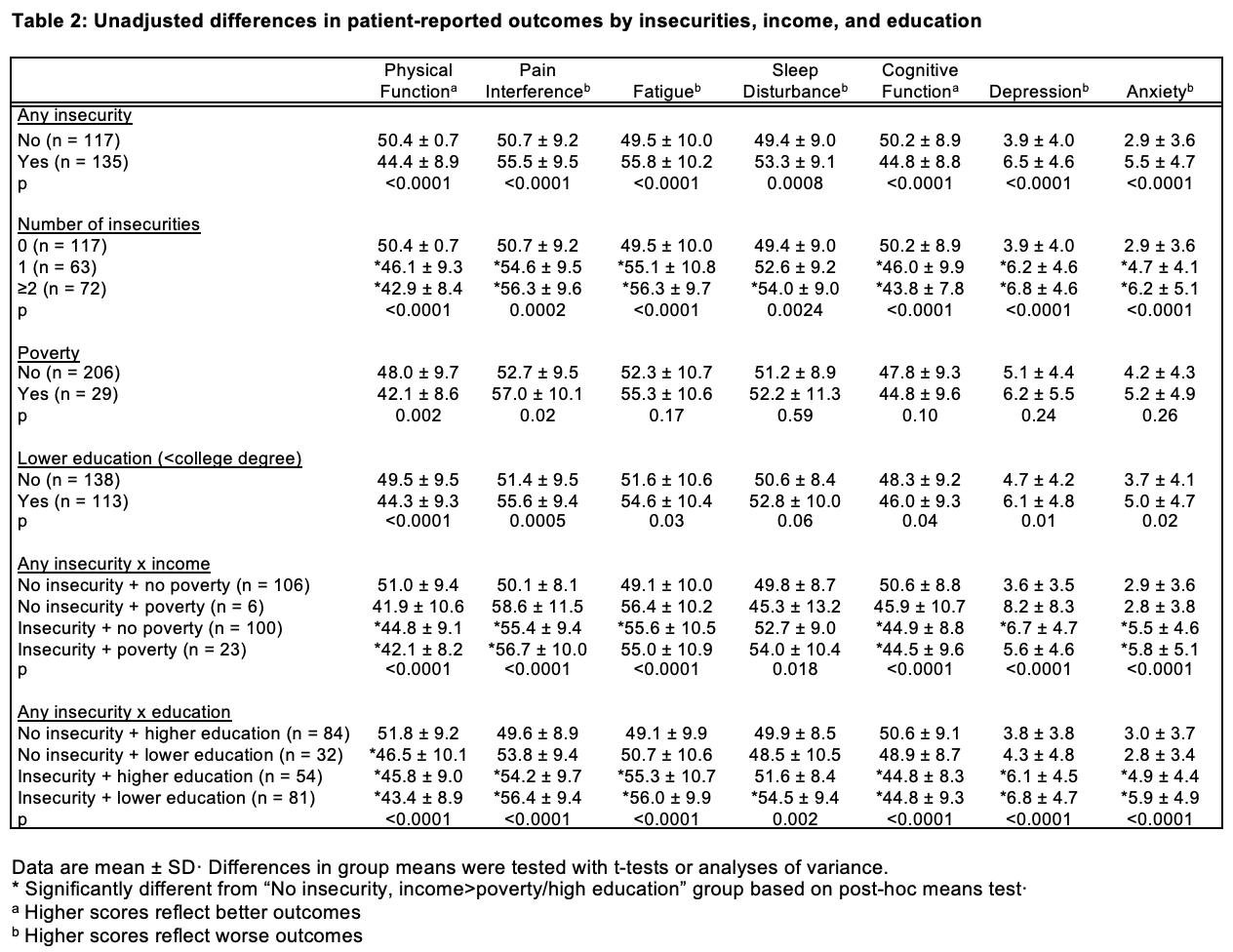
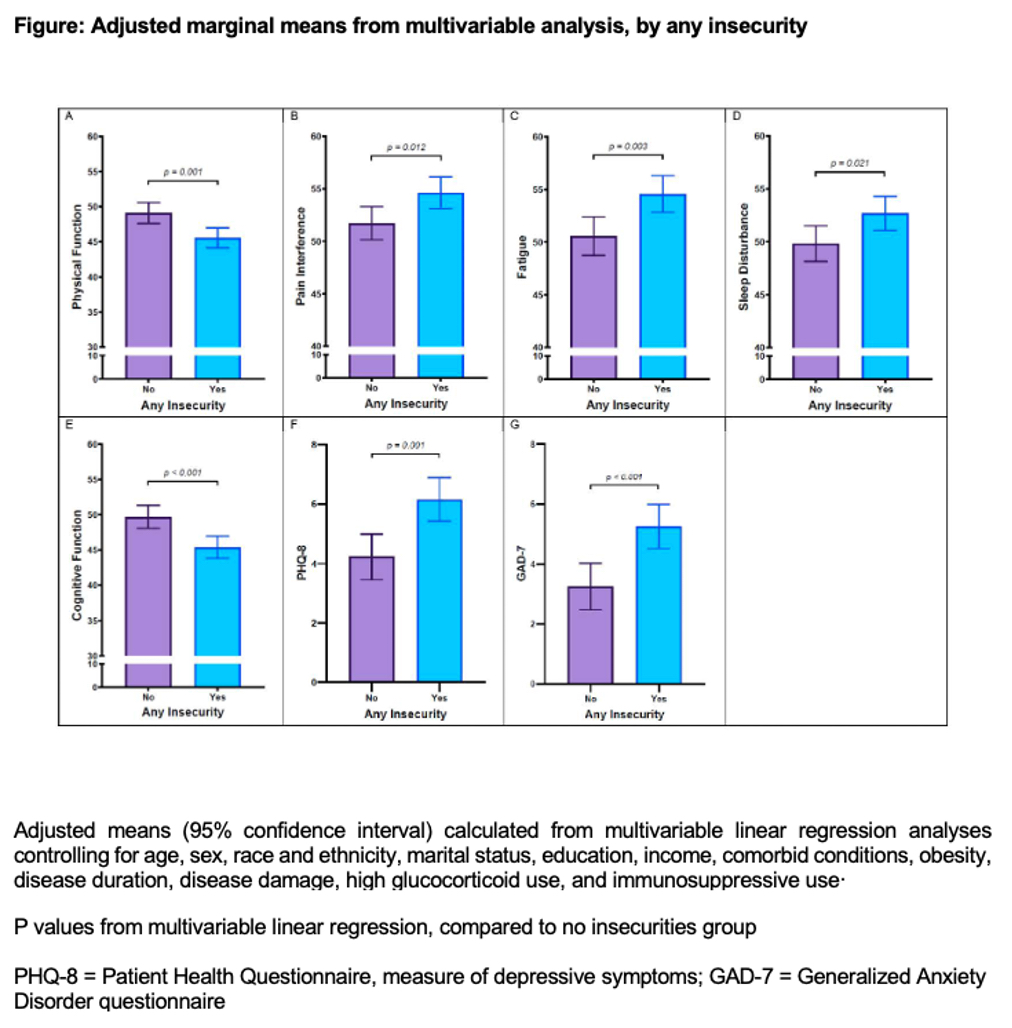
Results: Among 252 participants, 53.6% had at least one insecurity (Table 1). Insecurities were highly prevalent, and more common in those with poverty and lower education (79.3% vs. 44.8% of those with low vs. higher incomes, respectively, had any insecurities and 71.7% vs. 39.1% of those with lower vs. higher education, respectively, had any insecurities). Unadjusted analyses examining the relationship between material need insecurities and PROs revealed significant differences in all PROs between those with and without any material needs insecurity and by the number of insecurities. In the unadjusted models of the insecurity-poverty groups, overall significant differences between groups were noted for each PRO. In each case, the post-hoc means test after ANOVA analyses indicated differences between one or both insecurity groups (either “insecurity + no poverty” or “insecurity + poverty”) and the no insecurity + no poverty group. Similar results were noted for the insecurity-education group analysis (Table 2). Adjusted multivariate analyses revealed that participants with any insecurity had significantly worse scores across all PROs measured (Figure); individuals with more insecurities had worse PROs. There were no statistically significant interactions between insecurities and poverty or education.
Conclusion: Having any material need insecurity was associated with worse outcomes for patients with SLE regardless of poverty or education. Findings provide insight into mechanisms by which social risk factors can affect SLE outcomes and underscore the need for provider awareness of these modifiable factors and knowledge of relevant resources for interventions.
To cite this abstract in AMA style:
Sandoval-Heglund D, Roberts E, Park J, Dall'Era M, Barbour K, Lanata C, Greenlund K, Gordon C, Katz P, Yazdany J. Material Need Insecurities Are Associated with Worse Patient-Reported Outcomes Among Individuals with SLE [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/material-need-insecurities-are-associated-with-worse-patient-reported-outcomes-among-individuals-with-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/material-need-insecurities-are-associated-with-worse-patient-reported-outcomes-among-individuals-with-sle/