Session Information
Session Type: Abstract Submissions (ACR)
Multipotent mesenchymal stem cells (MSCs) are critical for bone and cartilage repair but the role of such cells in vivo in hip OA is poorly defined. Subchondral bone changes depicted as bone marrow lesions (BMLs) on MRI are intimately linked to joint remodelling and OA structural deterioration, suggesting potential aberrant MSC responses within such tissue. We hypothesised that deficiencies in native in vivo CD45–CD271+ MSC numbers and/or function contributed to BML pathophysiology and investigated BML and non-BML hip subchondral bone for numerical, topographic and in vitro functional differences.
Methods
Twenty femoral heads were obtained during total hip arthroplasty from subjects with primary hip OA that fulfilled the ACR criteria for hip OA. Ex vivo 3T MRI identified BML and non-BML regions from excised hips; one half was enzymatically treated to extract cells and the other half EDTA-decalcified to quantify trabecular bone area and cartilage thickness. Digital imaging was performed on 15 paired excisions using 92 manually defined morphologically homogenous regions containing cartilage and 188 regions containing only bone. The MSC frequency relative to total live cells was established using flow cytometry for the CD45–CD271+ phenotype. A colony forming unit-fibroblast (CFU-F) assay determined the number of MSCs per million cells. In vitro tri-lineage MSC differentiation assessed functional capacity of expanded CD271+ cells. MSC topography was examined using anti-CD271 IHC.
Results
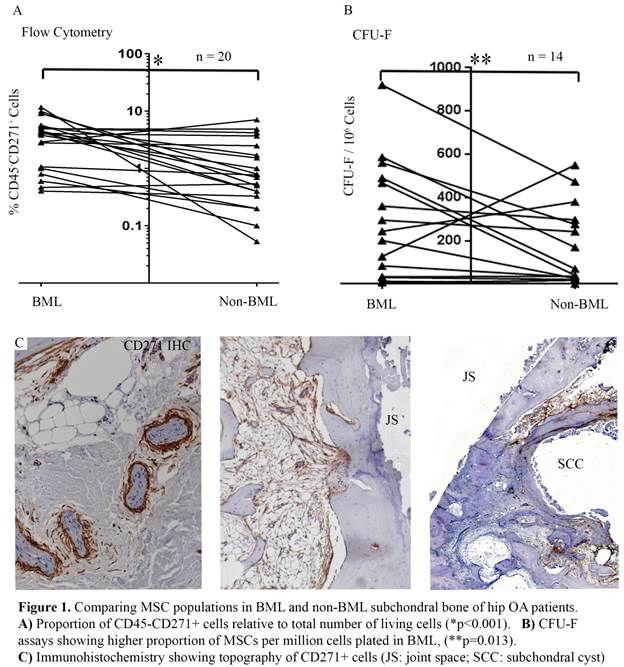
Regions with a normal appearance of cartilage were closely associated with non-BML excisions (p=0.01) compared to BML where most of the surface was damaged. Trabecular bone area was increased in BML regions (p=0.001). In 18/20 subjects, the proportion of native CD45–CD271+ MSC phenotype cells was higher in BMLs (Figure 1A, median 3.5-fold difference; p<0.001). This was confirmed using CFU-F assays (Figure 1B, 12/14 subjects, median 3.5-fold; p=0.013). Small differences were detected in MSC proliferation and mineralization capacities but not in their phenotype (>95% CD73+CD90+). We observed abundant CD271+ MSCs surrounding subchondral blood vessels near the cement line underlying cartilage lesions and in regions surrounding subchondral cysts, suggesting an accumulation and/or local proliferative MSC response to tissue injury (Figure 1C).
Conclusion
BMLs of OA femoral heads contain a higher proportion of MSCs with similar in vitro functional capacity compared to neighbouring non-BML regions. Topographically, MSCs appear to be abundant in areas of active osteochondral repair and neo-angiogenesis. Despite this abundance, the in vivo MSC response is likely to be inadequate in the face of abnormal joint biomechanical stressing. These data advocate that, given their abundance, in vivo MSC repair-capacity optimization may be a target for future OA treatments.
Disclosure:
T. M. Campbell,
None;
F. Ponchel,
None;
A. Gomez,
None;
R. J. Hodgson,
None;
D. McGonagle,
None;
P. G. Conaghan,
None;
E. Jones,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/markedly-increased-mesenchymal-stem-cell-activity-in-mri-bone-marrow-lesions-compared-with-non-involved-bone-in-osteoarthritic-hips/