Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Accelerated knee osteoarthritis (AKOA) is a painful disorder and is associated with several risk factors and pre-radiographic structural features. While no single factor can accurately predict who is at risk for AKOA, it would be beneficial to recognize the combinations of factors that identify adults at risk for AKOA. We examined the benefit of adding magnetic resonance (MR)-based features to clinical and demographic characteristics for classifying adults who develop AKOA.
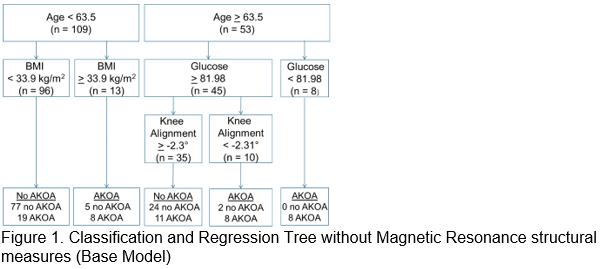
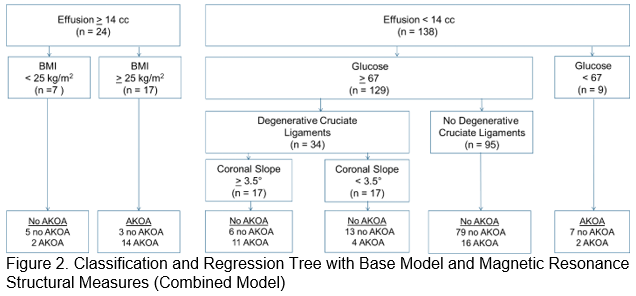
Methods: We conducted a case-control study using Osteoarthritis Initiative data from baseline and the first 4 annual visits. Eligible participants had no radiographic KOA in either knee at baseline (Kellgren-Lawrence [KL]<2). We classified 2 sex-matched groups: 1) AKOA: ≥1 knee developed advance-stage KOA (KL=3 or 4) within 48 months and 2) did not develop AKOA within 48 months. MR images were assessed at OAI baseline for 3 quantitative measures (effusion-synovitis volume, cartilage damage, and bone marrow lesion volume) and 9 semi-quantitative features (cruciate/collateral ligaments, extensor mechanism, gastrocnemius tendon, synovitis, medial/lateral meniscal pathology, medial/lateral meniscal effusion) that were read by two musculoskeletal radiologists. We performed 2 classification and regression tree (CART) analyses to determine classification rules and important variables for 1) a base model with baseline clinical (serum and radiographic measures) and demographic (age, sex, body mass index [BMI]) characteristics and 2) a combined model with baseline MR-based features in addition to the variables in the base model. Pruning and 10-fold cross-validation were performed to avoid overfitting.
Results: The most important variables for classifying individuals with incident AKOA in the base model (in order of importance) were age, serum glucose, and body mass index [BMI] (Figure 1). The most important variables in the combined model were effusion, serum glucose, presence of degenerative cruciate ligaments, and coronal tibial slope (Figure 2). The base model explained 31% of the variance, while the combined model explained 39% of the variance. Both the base and combined models offered good specificity (0.94 and 0.90) and moderate sensitivity (0.44 and 0.59, respectively).
Conclusion: MR-based features help classify adults who will develop AKOA; however, the cost of collecting standard MR-based features may outweigh the incremental improvement in classification in some settings.
To cite this abstract in AMA style:
Price LL, Harkey M, Ward RJ, MacKay J, Zhang M, Davis J, McAlindon TE, Lo GH, Amin M, Eaton CB, Lu B, Duryea J, Barbe M, Driban JB. Magnetic Resonance Imaging Features Can Classify Adults Who Will Develop Accelerated Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/magnetic-resonance-imaging-features-can-classify-adults-who-will-develop-accelerated-knee-osteoarthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/magnetic-resonance-imaging-features-can-classify-adults-who-will-develop-accelerated-knee-osteoarthritis/