Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Minority patients with systemic lupus erythematosus (SLE) experience a higher disease burden and encounter more barriers to care than White patients, resulting in worse outcomes and increased healthcare utilization. A Lupus Patient Navigator Program (LPNP) has been associated with improved SLE disease activity and quality-of-life scores in minority populations. This study aims to evaluate the impact of an LPNP on adherence to medication and scheduled visits.
Methods: Self-identified minority patients with SLE aged >18 years were recruited from an academic center. Inclusion criteria included being prescribed ≥1 immunosuppressant and meeting at least one of the following: 1) ≥1 missed clinic or laboratory visit in the past 6 months, 2) nonadherence to medical therapy, or 3) newly diagnosed SLE. The LPNP was modeled after the CDC STEPS to CARE toolkit. Patients engaged with the patient navigator every 3 months over a 12-month period via phone or in-person, with real-time resource support. Patient-reported outcomes included a medication diary, with adherence defined as the ratio of pills taken to pills prescribed over the week prior to each navigator encounter. Rheumatology visit adherence (in-person or telehealth) was tracked through chart review.
Results: Twenty-five patients (96% female; 92% Black; 8% Hispanic or Latino; mean age 32 years) completed the 12-month program. Among these, 92% were high school graduates, 88% had health insurance, and 48% were unemployed or disabled (Table 1). There was no statistically significant difference in visit adherence when comparing the year prior to LPNP enrollment to the LPNP period (Figure 1), with the exception of 2020 when missed visits increased (2019 p=0.63; 2020 p=0.05; 2021 p=0.81). During the study period, 52% of participants reported glucocorticoid use and 96% reported hydroxychloroquine (HCQ) use, with an average of 1.7 immunosuppressive medications per patient (Table 1). Medication adherence over the 12-month period (Figure 2) appeared to vary by medication type: adherence to injectable therapies declined, while adherence to oral agents—including DMARDs, hydroxychloroquine, and glucocorticoids—remained relatively stable.
Conclusion: The COVID-19 pandemic led to a peak in missed rheumatology visits among the high-risk patients with SLE participating in the LPNP. There appears to be mitigation of barriers with the LPNP in 2019, however missed visits increased in 2020 and 2021 despite the LPNP intervention. This may reflect a higher number of scheduled visits overall due to more frequent healthcare touchpoints introduced by the program. Tailoring navigator interventions to address the specific barriers associated with different treatment modalities—particularly injectable therapies—may enhance effectiveness. Further research is warranted to optimize navigator-based strategies and assess long-term outcomes in the context of evolving healthcare delivery challenges.
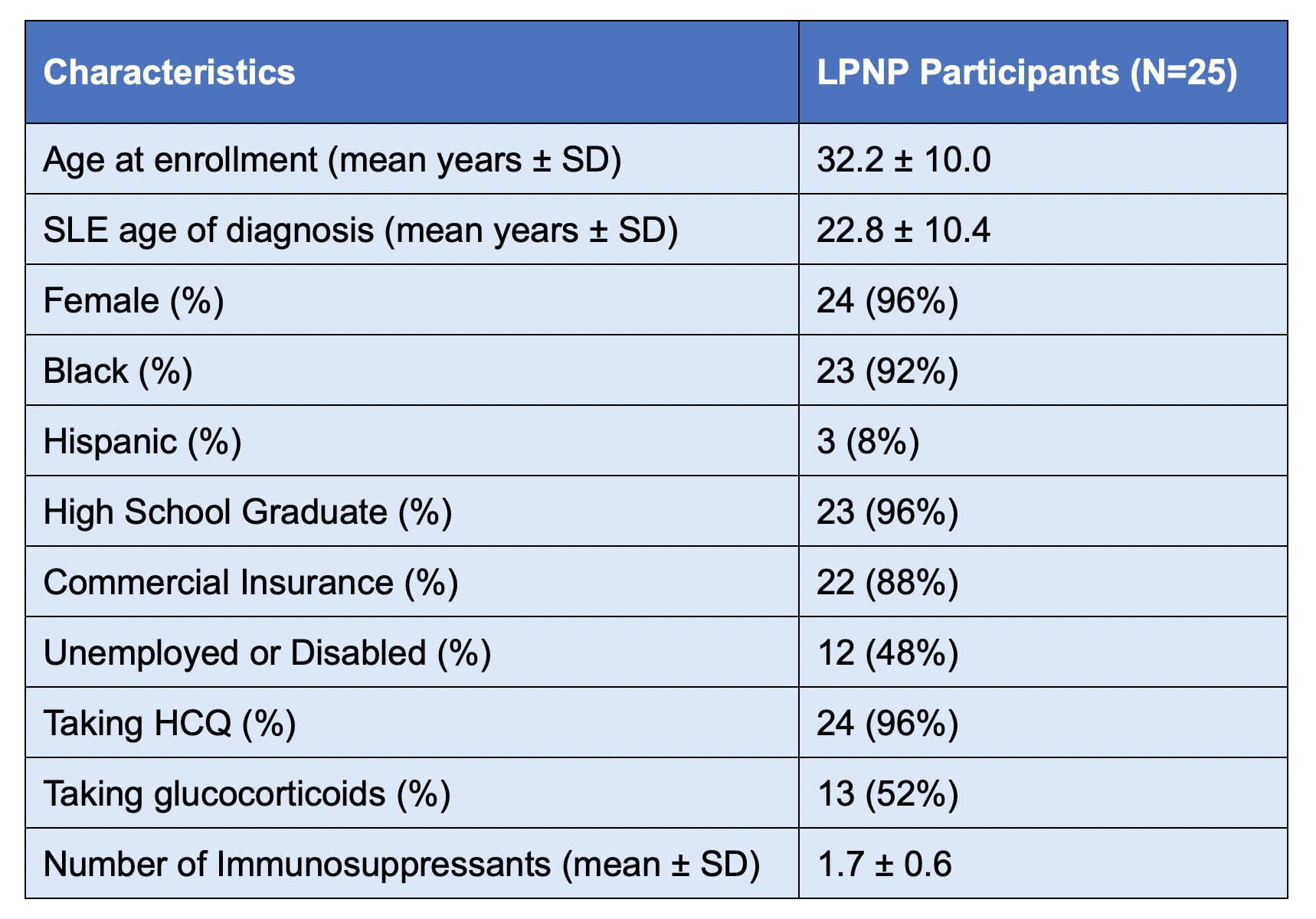 Table 1. Baseline LPNP Participant Characteristics
Table 1. Baseline LPNP Participant Characteristics
.jpg) Figure 1. Number of Missed Rheumatology Visits by Year
Figure 1. Number of Missed Rheumatology Visits by Year
.jpg) Figure 2. Adherence by Type of Medication Over 12 Months of LPNP Participation. cDMARD = conventional DMARD
Figure 2. Adherence by Type of Medication Over 12 Months of LPNP Participation. cDMARD = conventional DMARD
To cite this abstract in AMA style:
Vora R, Karim S, Wilson D, Singh J, Gilkeson G, Oates J, Kamen D. Lupus Patient Navigator Program for Improving Care Adherence for Minority Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/lupus-patient-navigator-program-for-improving-care-adherence-for-minority-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-patient-navigator-program-for-improving-care-adherence-for-minority-patients/
