Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: While medical comorbidities increase with age, younger age at onset of Systemic Lupus Erythematosus (SLE) has been associated with greater risk of some types of end-organ damage. Few studies have reported damage-free survival by age at diagnosis which would be useful for prognosis discussions. Using a large single-center retrospective cohort of incident SLE patients, the objectives of this study were to estimate new damage and mortality-free median survival time and 1-, 5-, and 10-year survival probabilities and to compare damage-free survival by age at diagnosis and within organ systems.
Methods: Electronic Health Records (EHR) from a single academic health system were queried for patients with SLE diagnosis codes in 2003-2016 and at least one visit to both a rheumatology and a primary care provider to better capture damage events. Trained abstractors manually validated cases meeting either 1997 ACR or 2012 SLICC SLE criteria and recorded damage event dates, including events pre-EHR. Age at diagnosis used the earliest date of a SLE diagnosis code from a rheumatologist or date of meeting SLE criteria. Patients with less than 30 days of observation after diagnosis were excluded.
All observed events within the post-diagnosis follow-up period were compared by age group at diagnosis (< 30, 30-44, 45-59, and 60+ years). Gross damage rates were calculated using Poisson regression. Kaplan-Meier was used to estimate new damage and mortality-free median survival time and 1-, 5-, and 10-year survival probabilities by age group at diagnosis. Differences in organ-specific damage-free survival by age group at diagnosis were assessed with logrank tests on Kaplan-Meier curves.
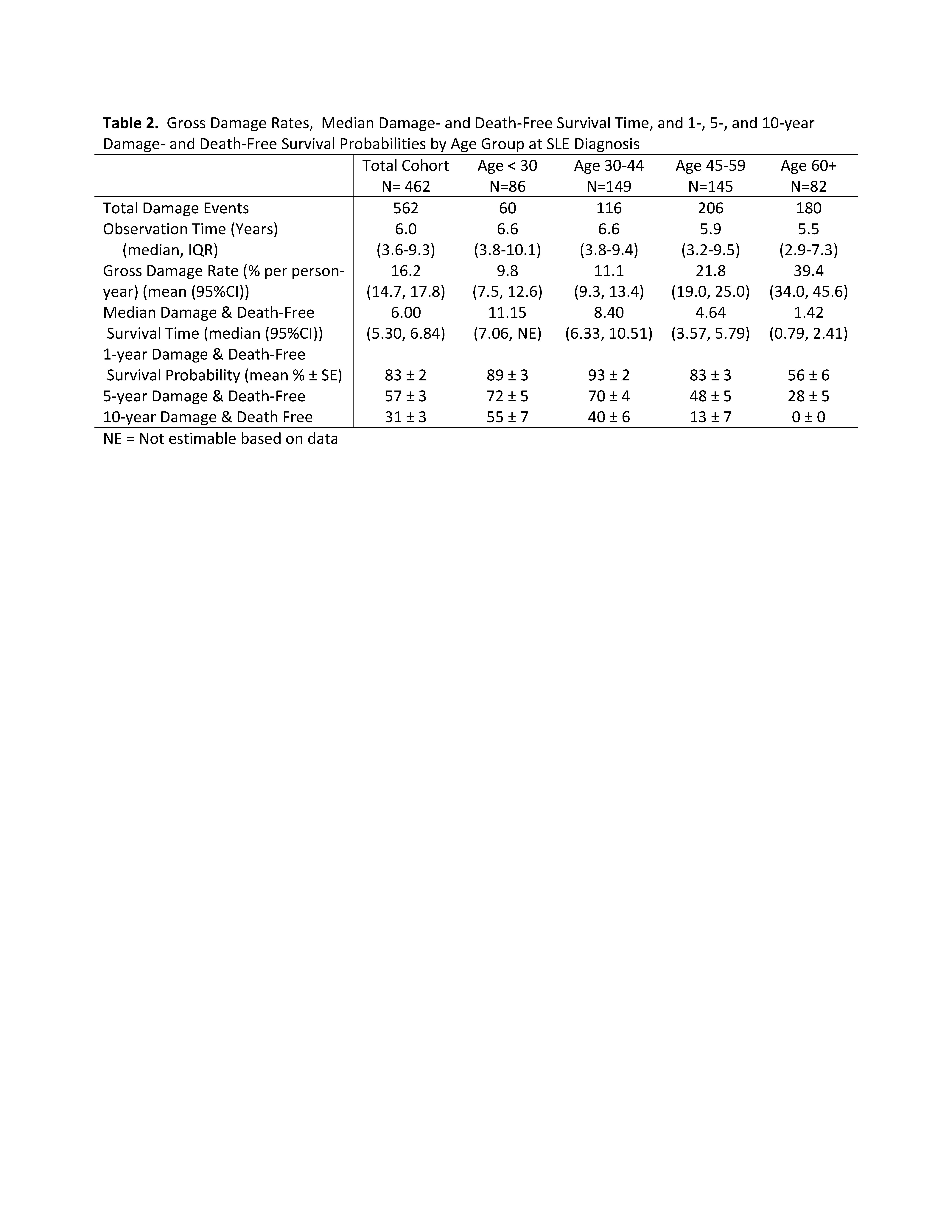
Results: The cohort included 462 patients with incident SLE followed for a median of 6 years. There were 86 (19%) patients diagnosed before age 30, and the median diagnosis age was 45 (Table 1). Patients diagnosed before age 30 were more likely to be Asian, Black or to receive Medicaid. Of SLE damage events observed after diagnosis, the most common were neuropsychiatric (18% of events), ocular (17%), and musculoskeletal (14%). Increasing age group correlated with gross damage rate, from 10% per year risk in those < 30, to 39% per year risk in those 60+ (Table 2). Survival until first damage event after diagnosis was similar in patients diagnosed before age 30 and ages 30-44; survival decreased in older age groups. In the first year, patients younger than 30 years experienced damage rates similar to older age groups (45-59 year olds) (Figure 1). For most organ systems, survival without damage negatively correlated with age. However, cardiovascular and pulmonary damage-free survival was similar or shorter in patients diagnosed < 30 compared to those diagnosed decades later in life.
Conclusion: Younger patients (< 30), who were more likely to be non-White and Medicaid beneficiaries, experienced a relatively high rate of first damage in the first year after diagnosis and similar damage rates to patients decades older within cardiovascular and pulmonary systems. Overall damage rates in SLE correlated with age at diagnosis, with a 30% per year difference in damage risk between the youngest (< 30) and oldest ( >60) patients at SLE diagnosis.
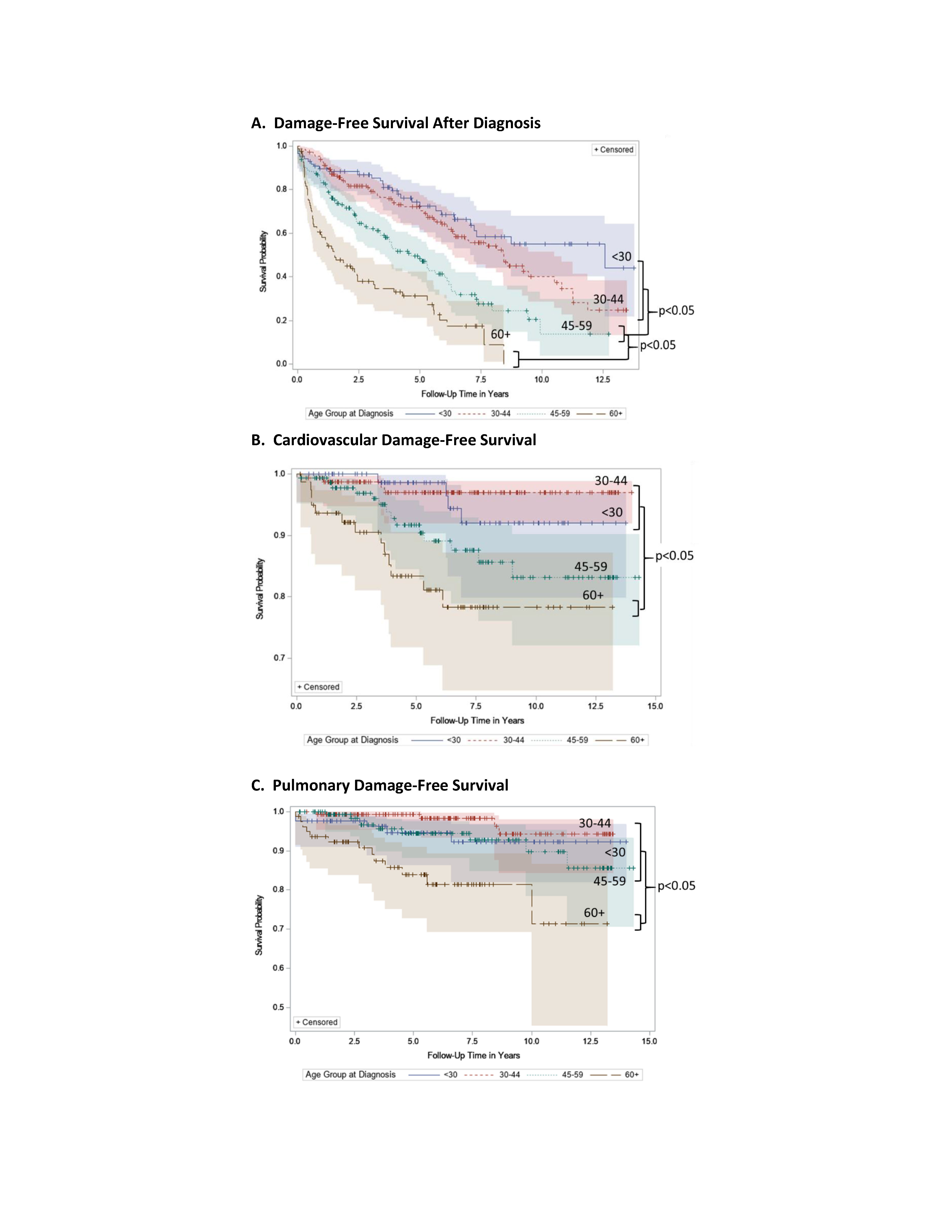 Figure 1. Damage, Cardiovascular, and Pulmonary Damage-Free Survival by Age Group at Diagnosis. Kaplan-Meier survival curves for damage after lupus diagnosis by age group at diagnosis with death as a censoring event for select organ systems. Panel A shows survival until first new damage event after diagnosis. Survival time was longer in patients diagnosed before age 45 and decreased with increasing age group. Panel B shows cardiovascular damage-free survival, which was longer for patients diagnosed before 45 compared to those after age 60. Panel C displays pulmonary damage-free survival which was shorter for patients diagnosed after age 60 than those diagnosed younger.
Figure 1. Damage, Cardiovascular, and Pulmonary Damage-Free Survival by Age Group at Diagnosis. Kaplan-Meier survival curves for damage after lupus diagnosis by age group at diagnosis with death as a censoring event for select organ systems. Panel A shows survival until first new damage event after diagnosis. Survival time was longer in patients diagnosed before age 45 and decreased with increasing age group. Panel B shows cardiovascular damage-free survival, which was longer for patients diagnosed before 45 compared to those after age 60. Panel C displays pulmonary damage-free survival which was shorter for patients diagnosed after age 60 than those diagnosed younger.
To cite this abstract in AMA style:
Schletzbaum M, Ezeh N, McKown T, Garg S, Bartels C. Lupus Damage Free-Survival by Age at Diagnosis: A Retrospective Incident Lupus Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lupus-damage-free-survival-by-age-at-diagnosis-a-retrospective-incident-lupus-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-damage-free-survival-by-age-at-diagnosis-a-retrospective-incident-lupus-cohort/