Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Interstitial lung disease (ILD) is a frequent and severe complication of rheumatoid arthritis (RA) and systemic sclerosis (SSc). Although computerized tomography (CT) is considered the gold-standard for diagnosis, lung ultrasound (LUS) has recently emerged as a diagnostic technique in the assessment of ILD. The aim of the present study is to evaluate the usefulness of LUS in the assessment of ILD in patients with RA and SSc.
Methods: A single-center, cross-sectional study was performed in patients with RA and SSc who had an indication for chest CT as a screening, diagnostic or follow-up technique for ILD. A lung CT and LUS were performed on the same day. LUS was performed with a 6-10 mHz linear probe. Two LUS were performed, in the first one the B-lines were counted in the 14 spaces defined by Gutierrez et al, and in the second one the pleura was evaluated according to the criteria of Fairchaild et al. In addition, maximal pleural thickness was measured in the subscapular spaces. Pulmonary function tests (PFT) were performed in the 2 months adjacent to the CT scan. Two-sample comparisons were performed using a t-test or Mann–Whitney U test. Parametric Pearson or non-parametric Spearman correlation coefficient analyses were used to test the correlation between parameters, as appropriate. Area under the curve (AUC),sensitivity and specificity were calculated for the LUS scores.
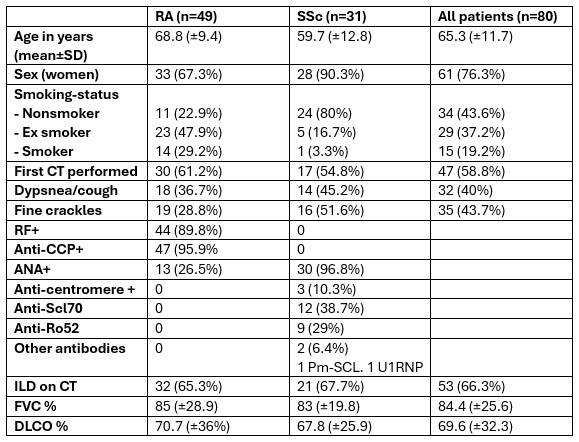
Results: Eighty patients were enrolled, 49 patients with RA and 31 with SSc (Table 1). A total of 53 patients (66.3%) had ILD according to CT. The mean time to perform lung ultrasound for the B-line and the pleural assessment was 09:15 and 07:45 minutes, respectively.
There was a significant correlation between the presence of ILD with the B-line score (p< 0.001) and pleural score (p< 0.001). There was also a significant correlation between pleural thickness at lung bases and the presence of ILD (2.41 mm vs 0.91 mm, p< 0.001).
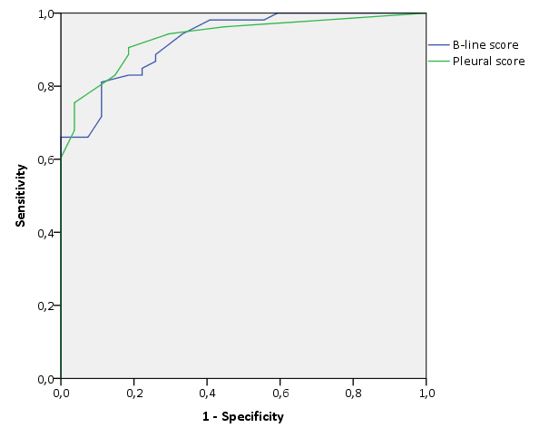
There was a moderate correlation between B-line count with FVC (-0.42, p< 0.001) and DLCO (-0.43, p< 0.001). The pleural score had a low correlation with FVC (-0.27, p=0.016) and moderate correlation with DLCO (-0.49, p< 0.001). The AUC for B lines was 0.926 (Figure 1). The optimal cutoff point for the diagnosis of ILD was > 10 B lines, with a sensitivity of 0.81 and a specificity of 0.89. The AUC for pleural alterations was 0.933 (Figure 1). The optimal cutoff point was > 2 pathologic pleural spaces, with a sensitivity of 0.91 and a specificity of 0.81.
There was a significant association between the presence of honeycombing on chest CT at bases and maximum pleural thickness measured by ultrasound, being statistically significant in the right base (4.29 mm vs. 1.64 mm, p< 0.001), although it did not reach statistical significance in the left base (3.27 mm vs. 1.54mm, p=0.16).
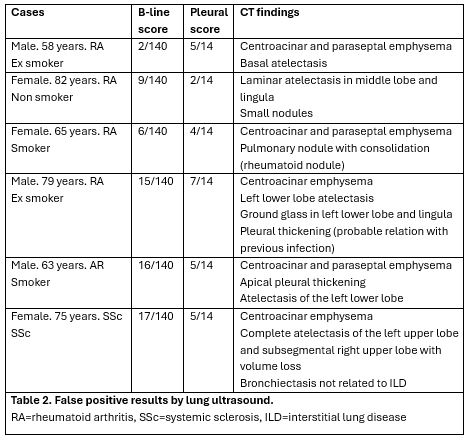
The CT scans of patients with false positive results by LUS were reviewed, finding CT alterations that justified the findings (table 2).
Conclusion: LUS seems to be a useful technique in the diagnosis of ILD in RA and SSc, presenting good sensitivity and specificity, as well as a moderate correlation with the PFT. Pleural assessment is less time consuming and have a higher diagnostic yield compared to B-line counting.
To cite this abstract in AMA style:
Loarce J, García de Vicente A, Arechavala Hita J, de La Puente Bujidos C, Rigual J, Bachiller Corral F, Vázquez Díaz M. Lung Ultrasound in Rheumatoid Arthritis and Systemic Sclerosis: Accuracy of B-line and Pleural Assessment [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/lung-ultrasound-in-rheumatoid-arthritis-and-systemic-sclerosis-accuracy-of-b-line-and-pleural-assessment/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lung-ultrasound-in-rheumatoid-arthritis-and-systemic-sclerosis-accuracy-of-b-line-and-pleural-assessment/