Session Information
Session Type: ACR Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Systemic autoimmunity associated with RA precedes the onset of inflammatory arthritis (IA) by several years. In particular, the presence of systemic anti-cyclic citrullinated peptide (CCP) antibody is a strong predictor of developing classified RA in the future. However, the mechanisms involved in the transition from systemic anti-CCP to IA classifiable as RA are unknown. Our group has previously identified the local generation of anti-CCP and rheumatoid factor (RF) antibodies in the sputum of subjects at-risk for RA, including those with serum anti-CCP positivity. It has also been demonstrated that a portion of serum anti-CCP+ individuals have chronic lung disease preceding joint disease in RA. Herein, we aimed to determine the relationship between lung-related factors and the transition from systemic autoimmunity to classified RA.
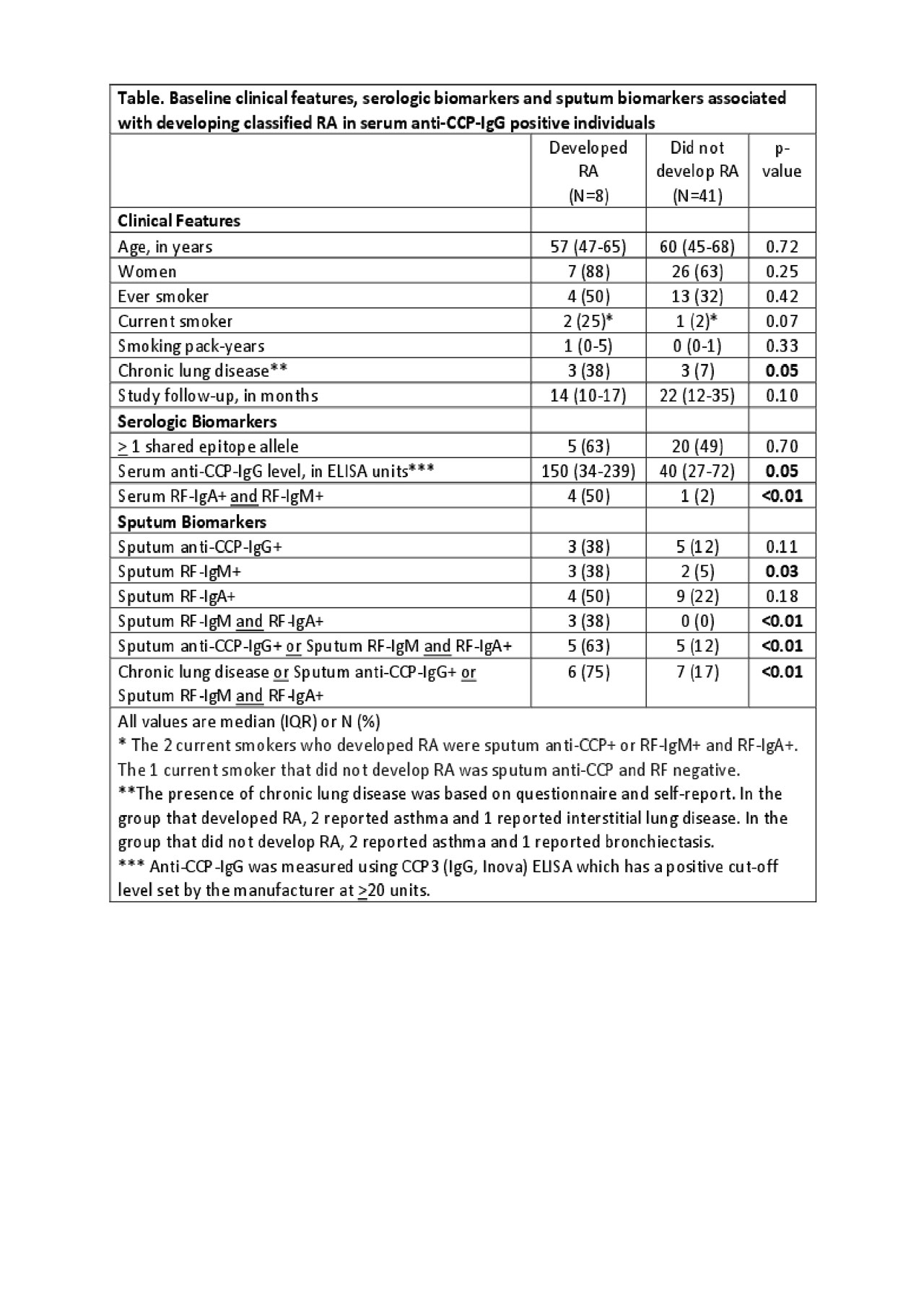
Methods: In 49 subjects who were serum anti-CCP-IgG+ without IA, we collected baseline induced sputum using hypertonic saline. Baseline serum and sputum supernatant were tested by ELISA for CCP-IgG (CCP3, Inova), RF-IgM (Inova) and RF-IgA (Inova). Sputum antibody positivity was defined as a level above the 95th percentile in values determined from a separate cohort of 80 serum anti-CCP negative controls without IA. All subjects were followed longitudinally up to 3 years. Incident RA was determined by 2010 ACR/EULAR classification criteria. Chi-square and Wilcoxon rank-sum testing was used to compare factors associated with incident RA.
Results: Eight (16%) of 49 subjects developed classified RA during follow-up (median time to RA 14 months). Factors associated with developing RA are listed in the Table. Similar to previous data, we found that higher serum anti-CCP-IgG level (p=0.05) and serum RF positivity (p< 0.01) were associated with developing RA. In addition, we also found multiple lung-related factors associated with developing classified RA, including a self-reported history of any chronic lung disease (OR=7.6, 95% CI 1.2-48.4), sputum positivity for anti-CCP-IgG or 2 RF isotypes (RF-IgA and RF-IgM) (OR=12.0, 95% CI 2.2-66.3) and a trend toward an association with current smoking (OR=13.3, 95% CI 1.0-170.6). Of note, both current smokers who developed classified RA had sputum autoantibody positivity. When considering these lung factors in aggregate, incident RA was 15 times more likely in subjects with sputum RA-related antibodies or chronic lung disease (OR=14.6, 95% CI 14.4-87.7).
Conclusion: In a cohort of serum anti-CCP+ subjects, we found that lung-related factors at baseline, including sputum anti-CCP, sputum RF isotypes and a history of chronic lung disease, were associated with developing classified RA within a short duration of follow-up (< 3 years). These data support that biological pathways in the lung may be important in transitions from systemic autoimmunity to arthritis in RA. Based on our findings, it will be particularly important to understand whether the generation of anti-CCP and RF in the lung is a mediating factor that links smoking and RA. In addition, 2 of 8 subjects who developed RA did not have sputum autoantibodies or chronic lung disease, which could suggest other mucosal site involvement in their transitions to RA.
To cite this abstract in AMA style:
Visser A, Feser M, Fleischer C, Lenis-Charry L, August J, Bemis E, Norris J, Holers V, Deane K, Demoruelle M. Lung-Related Factors Are Associated with Transitions from Systemic Anti-CCP Antibody Positivity to Classified RA [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/lung-related-factors-are-associated-with-transitions-from-systemic-anti-ccp-antibody-positivity-to-classified-ra/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lung-related-factors-are-associated-with-transitions-from-systemic-anti-ccp-antibody-positivity-to-classified-ra/