Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Incomplete SLE (iSLE) defines a group of patients with symptoms typical of SLE but not meeting sufficient criteria required for the classification of SLE. Up to 55% of patients with iSLE will eventually develop SLE, but it is unclear which patients are at risk of progression.(1) Neutrophil dysfunction, among which aberrant neutrophil extracellular trap (NET) formation driven by low density granulocytes (LDGs), has been implicated in SLE pathogenesis.(2) However, the role of neutrophil dysfunction in early forms of SLE is still unclear. Therefore, the aim of this study was to investigate whether LDGs are elevated in iSLE patients, compared to healthy controls (HCs) and SLE patients with quiescent disease (SLEDAI ≤ 4). Next to that, we investigated presence of circulating NETs in plasma of iSLE as well as SLE patients and HCs.
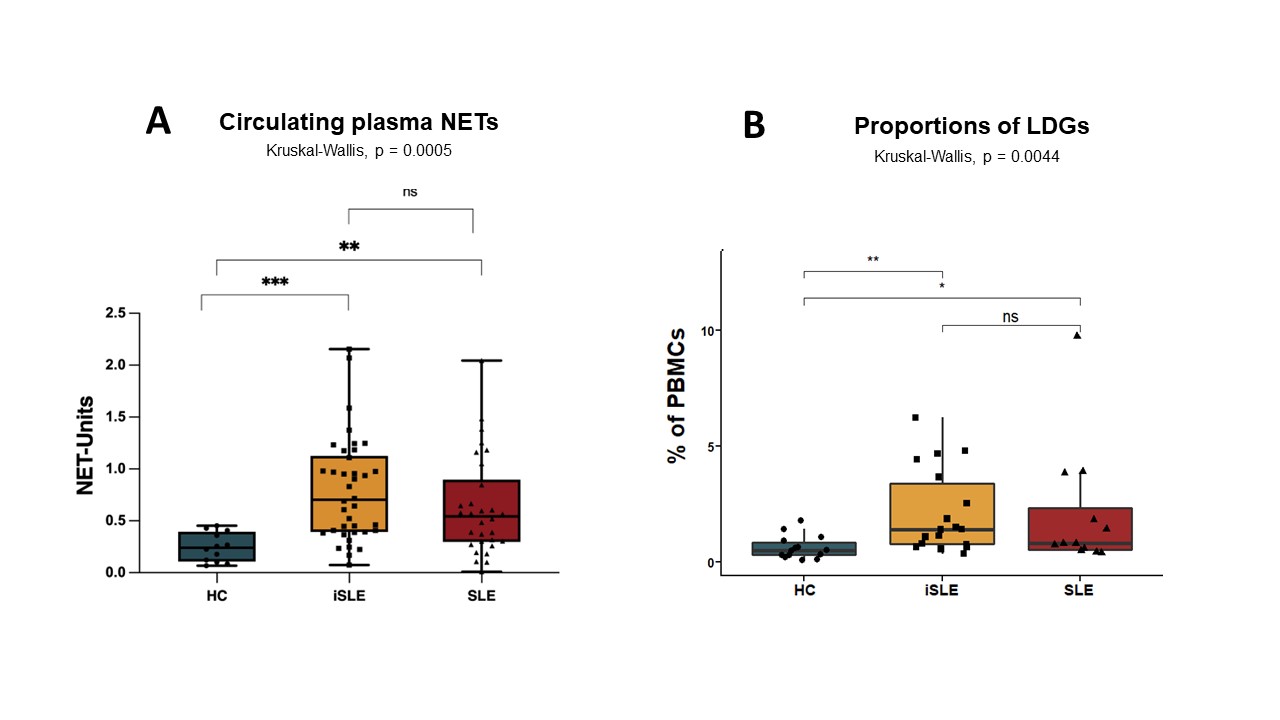
Methods: Circulating plasma NETs were measured cross sectionally in 38 iSLE patients, 30 SLE patients with quiescent disease and 12 HCs while LDGs were measured in 18 iSLE patients, 13 SLE patients and 14 HCs. SLE patients were classified according to the Systemic Lupus International Collaborating Clinics (SLICC) criteria. Patients with iSLE had to meet at least one clinical and one immunological criterion but less than four SLICC criteria in total. LDGs (CD14lowCD15+) were measured in freshly isolated PBMCs with flow cytometry and were expressed as percentage of total PBMCs. Circulating plasma NETs were measured with a sandwich enzyme linked immunosorbent assay using a plate coated with an anti-myeloperoxidase antibody.
Results: Proportions of LDGs and NET-levels were significantly increased in iSLE patients compared to HCs, as shown in Figure 1. The proportion of LDGs and circulating plasma NETs was similar between SLE and iSLE patients.
Conclusion: Our data shows significantly higher amounts of LDGs and circulating NETs in the iSLE and SLE cohort compared to healthy controls, suggesting that aberrant NET formation and clearance is present in early stages of the disease. In future studies, we aim to investigate the correlation between LDGs, circulating NETs and other immunological parameters, such as interferon signature, and anti-dsDNA levels.
(1) Lambers WM, Westra J, Bootsma H, de Leeuw K. From incomplete to complete systemic lupus erythematosus, A review of the predictive serological immune markers. Vol. 51, Seminars in Arthritis and Rheumatism. W.B. Saunders; 2021. p. 43–8.
(2) Kaplan MJ. Neutrophils in the pathogenesis and manifestations of SLE. Vol. 7, Nature Reviews Rheumatology. 2011. p. 691–9.3
To cite this abstract in AMA style:
Henning S, Reimers T, Doornbos-van der Meer B, Horvath B, Bootsma H, de Leeuw K, Westra J. Low-Density Granulocytes and Neutrophil Extracellular Traps in Incomplete Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/low-density-granulocytes-and-neutrophil-extracellular-traps-in-incomplete-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-density-granulocytes-and-neutrophil-extracellular-traps-in-incomplete-systemic-lupus-erythematosus/