Session Information
Date: Saturday, November 16, 2024
Title: Metabolic & Crystal Arthropathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Calcium pyrophosphate deposition (CPPD) disease is a crystalline arthritis affecting older adults. Systemic inflammation occurs during flares of acute calcium pyrophosphate (CPP) crystal arthritis but has not been well-studied in chronic CPPD. We investigated longitudinal patterns of C-reactive protein (CRP) values in patients according to CPPD phenotype.
Methods: In a prospective single-center registry of patients fulfilling ACR/EULAR 2023 CPPD Classification Criteria we reviewed the electronic health record (EHR) to categorize phenotypes according to EULAR 2011 terminology: acute CPP crystal arthritis only (acute CPP), chronic CPP inflammatory arthritis only (chronic CPP), or both acute & chronic CPP. Patients without documented joint inflammation were excluded. Acute flares were defined by ≥2 symptoms (swelling, warmth, tenderness, or pain), plus synovial fluid analysis positive for CPP crystals and/or chondrocalcinosis in the symptomatic joint and/or a rheumatologist documented a flare. We required ≥14 days between acute flares. Chronic symptoms were defined by ≥3 of 4 of chondrocalcinosis in symptomatic joint, worsened pain, worsened swelling, or requiring medication. Index date was the date of CPPD diagnosis (1st acute flare or 1st mention of CPPD). CRP (mg/L) was extracted from index date to 3/2024. We included patients with ≥1 CRP after index date and required ≥14 days between CRP values. When CRP >50 mg/L, we reviewed the EHR and excluded it if an alternate explanation was identified. We evaluated CRP distribution overall and by phenotype. Longitudinal CRP values were plotted in each group with restricted splines and 95% CI. Mixed effects models adjusted for age and sex estimated the effect of CPPD phenotype on CRP over time.
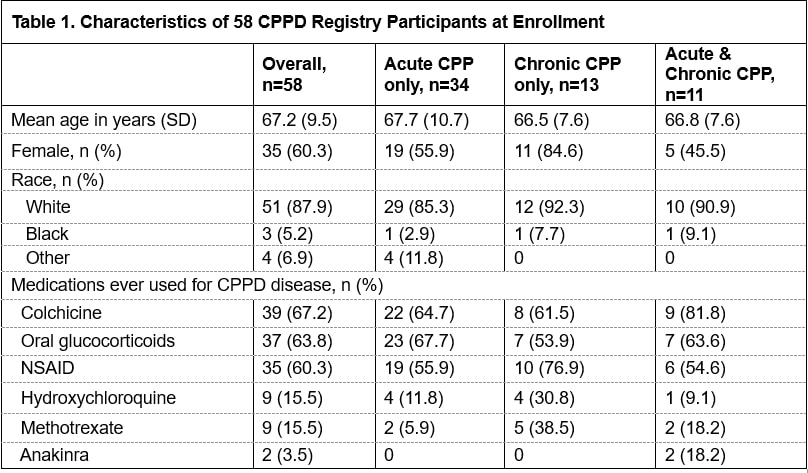
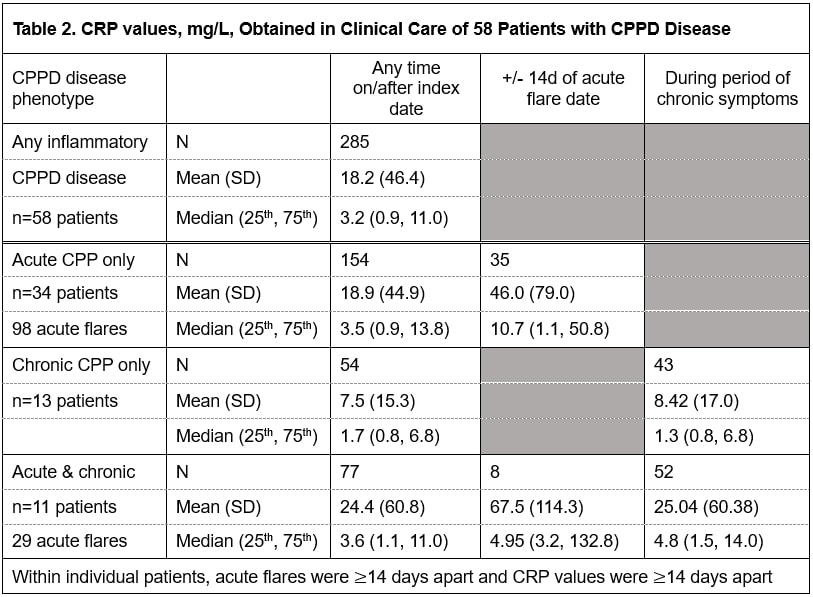
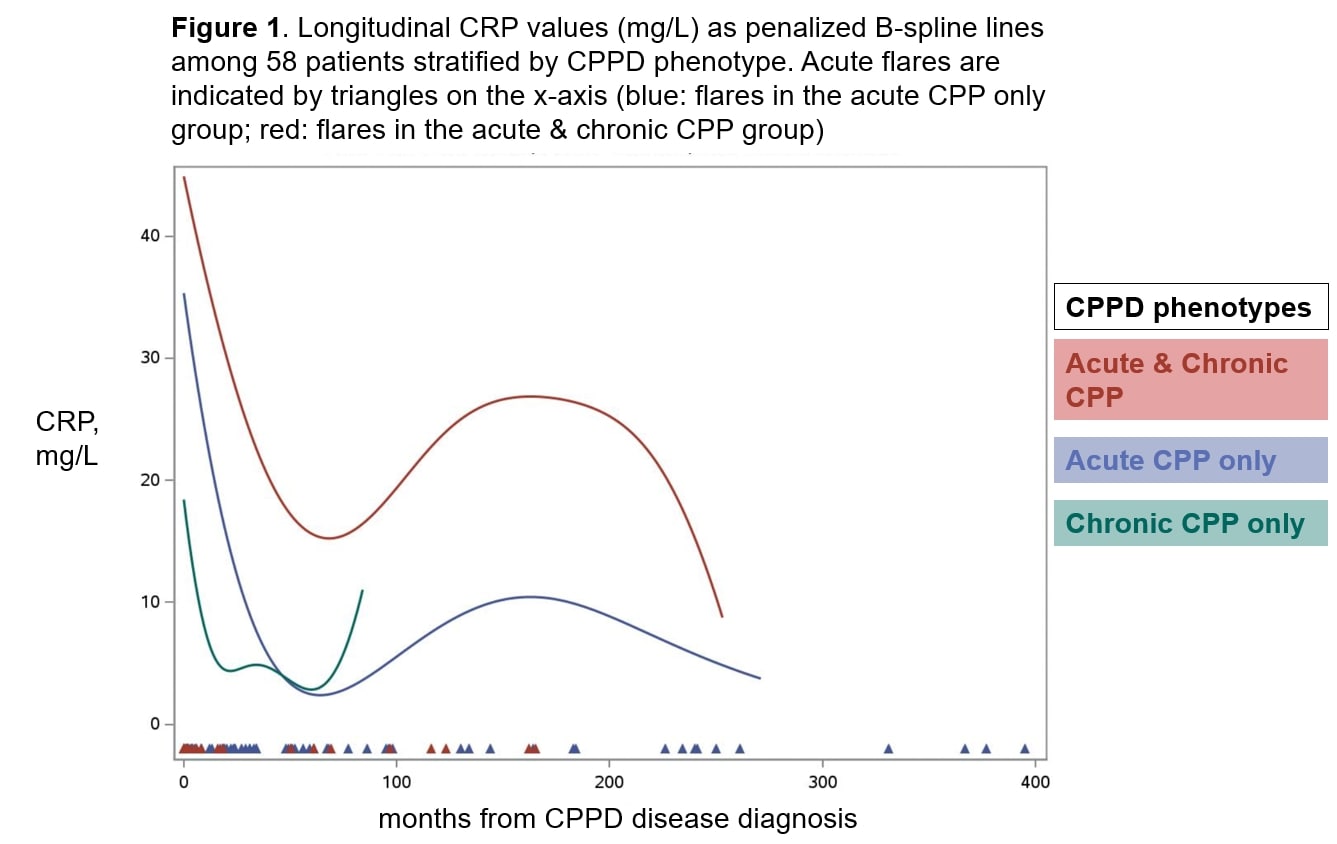
Results: Among 58 patients with 285 CRP values, mean age was 67 years, 60% female, 88% White (Table 1). CPPD phenotypes distributions were acute CPP only (59%), chronic CPP only (22%), acute & chronic CPP (19%). Colchicine (67%) and steroids (64%) were the most common treatments (Table 1). Mean CRP was 18.2 (46.36) mg/L and median CRP was 3.2 (0.9, 11.0) mg/L overall. CRP was tested within 14d of acute flare for approximately 1/3 of flares; in the 14d around flare, mean CRP was 46.0 (SD 79.0) mg/L in the acute CPP group and 67.5 (SD 114.3) mg/L in the acute & chronic group (Table 2). Longitudinal CRP values fluctuated most widely in the acute CPP group, and CRP was highest at the time of CPPD diagnosis in all three groups (Figure 1). CRP was non-significantly higher over time in the acute & chronic CPP group compared to chronic CPP (p=0.06), and higher in acute CPP than chronic CPP (p=0.14).
Conclusion: We identified distinct patterns of CRP obtained in clinical care according to CPPD disease phenotype, with the greatest fluctuation over time in patients with both acute & chronic CPP arthritis. CPPD treatments may have impacted CRP patterns, as anti-inflammatory treatments were common.
To cite this abstract in AMA style:
Gill M, Guan H, Collins J, Tedeschi S. Longitudinal Patterns of C-Reactive Protein Values in Calcium Pyrophosphate Deposition (CPPD) Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/longitudinal-patterns-of-c-reactive-protein-values-in-calcium-pyrophosphate-deposition-cppd-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-patterns-of-c-reactive-protein-values-in-calcium-pyrophosphate-deposition-cppd-disease/