Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with rheumatoid arthritis (RA) have an increased risk for developing cardiovascular diseases (CVD). This is partly due to the systemic inflammation characteristic to the disease, but also due to increased prevalences of ‘traditional’ risk factors such as dyslipidemia. The inflammation in RA often leads to an increased catabolism of lipids, resulting in decreases in HDL and LDL levels, while treatment with anti-inflammatory medication reverses these effects. The increased CVD risk with (very) low cholesterol levels appears contradictory and is referred to as the ‘lipid paradox’. Additionally, N-terminal pro-brain natriuretic peptide (NT-proBNP) is an independent predictor of CV morbidity and mortality, and is used in screening for congestive heart failure. Monitoring and interpretation of CVD surrogate markers or biomarkers in RA patients is challenging because they fluctuate along with disease activity, inflammatory burden and RA treatment. Therefore, the aim of the current study was to explore the changes in lipid and NT-proBNP levels in RA patients through different phases of the disease: from the preclinical stage and RA onset up to the treatment phase with (biological) DMARDs (bDMARDS).
Methods: Thirty-nine consecutive patients who were previously included in both Reade’s RA prevention cohort and biological cohort were included in the current study. The prevention cohort consisted of individuals with arthralgia and rheumatoid factor and/or anti-citrullinated protein antibodies without arthritis, and the biological cohort comprised RA patients using bDMARDs. Lipid spectrum and NT-proBNP levels were measured longitudinally and the following points in the disease course were identified in each patient (time from baseline was different in each patient due to the natural course of disease progression):
1. Baseline, months prior to RA diagnosis (Start RA-risk cohort)
2. Moment of RA diagnosis (End RA-risk cohort)
3. Period between diagnosis and start bDMARD treatment
4. Start treatment with bDMARDs
5-8. Continued treatment with bDMARDs
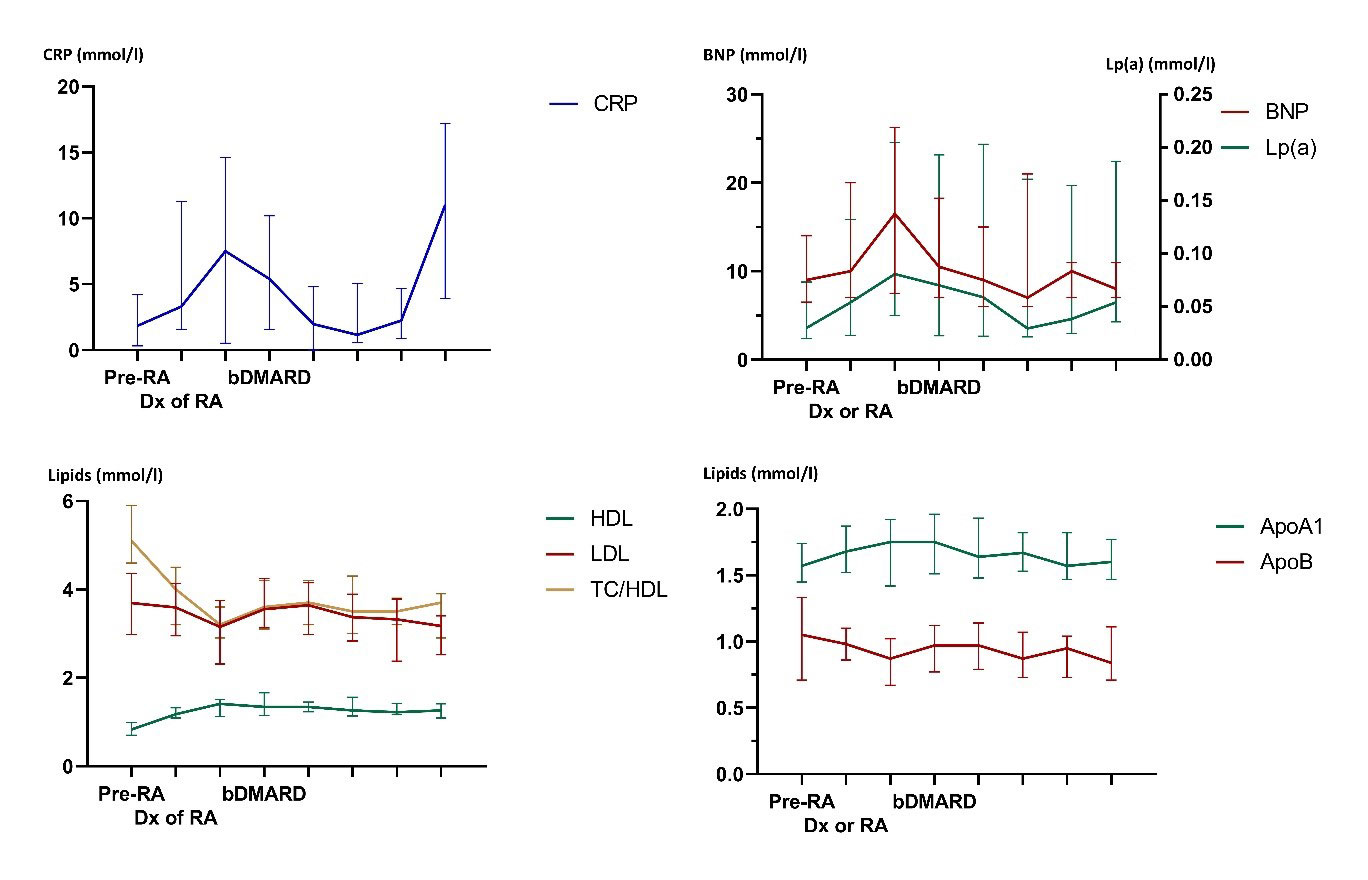
Results: From baseline, C-reactive protein (CPR) initially increased sharply, decreasing with the start of biological treatment and increasing again at end of follow up. Total cholesterol/high-density cholesterol (HDL) ratio, low-density cholesterol and apolipoprotein A1 decreased with rises in CRP, while HDL, lipoprotein (a), apolipoprotein B and NT-proBNP increased alongside CRP levels. Progression of all parameters is shown in Figure 1.
Conclusion: Our study uniquely shows the change of lipid parameters during the course of RA disease. Pro-atherogenic changes in lipid profile and NT-proBNP are associated with changes in inflammation. This process is already initiated before RA diagnosis, indicating the need for timely control of inflammation to optimize these parameters and thus optimizing CVD risk.
1 (n = 39), 2 (n = 25), 3 (n = 8), 4 (n = 36), 5 (n = 35), 6 (n = 25), 7 (n = 13), 8 (n = 9).
To cite this abstract in AMA style:
Raadsen R, van Boheemen L, Nurmohamed M. Longitudinal Lipid Profile and NT-proBNP Changes from Pre-clinical to Established Rheumatoid Arthritis: A 12 Years Follow up Explorative Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/longitudinal-lipid-profile-and-nt-probnp-changes-from-pre-clinical-to-established-rheumatoid-arthritis-a-12-years-follow-up-explorative-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-lipid-profile-and-nt-probnp-changes-from-pre-clinical-to-established-rheumatoid-arthritis-a-12-years-follow-up-explorative-study/