Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose : Longitudinal data on the type, progression, and predictors of arterial lesions in patients with Takayasu’s arteritis (TAK) is limited. This study aimed to characterize lesions of large arteries in patients with TAK and identify predictors of new lesions.
Methods: Clinical, laboratory, and imaging data from patients with TAK enrolled in a prospective, multicenter, longitudinal study and/or a randomized clinical trial were included in this study. Lesions were defined as “new or worse” or “improved” arterial aneurysm, stenosis, or occlusion as determined by angiography (83% Magnetic Resonance Angiogram, 23% Computerized Tomography Angiogram, and 4% Conventional Angiogram). Clinical features were defined as the presence of any symptom or sign attributed to vasculitis. Logistic regression was used to analyze the association of baseline (visit 1) variables with new/worse or improved lesions.
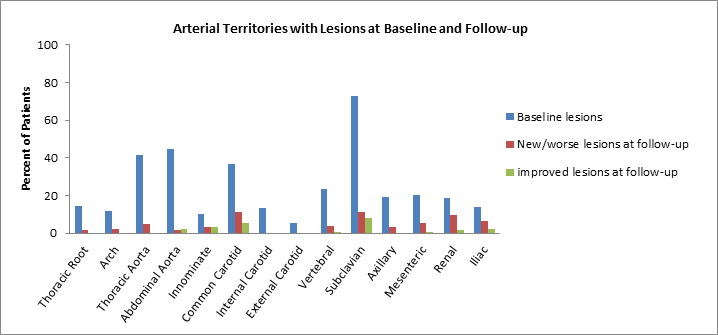
Results : The study included 175 patients with TAK: 93% female, 85% Caucasian, mean (±SD) age at diagnosis = 34.4±13.4 years, and mean (±SD) follow-up = 3.8±3.1 years. At baseline, the most frequently affected arteries were subclavian (73% of patients), abdominal aorta (44%), thoracic aorta (42%), and common carotid (37%) (Figure 1). In 123 patients with serial imaging, new or worse arterial lesions were noted in 35 patients (28%) predominantly in the subclavian, common carotid, renal, and iliac territories. 96 % of patients with new lesions were either on prednisone and/or other immunosuppressive agents. Improved stenotic lesions, mostly of the subclavian and common carotid arteries, were noted in 16 patients (13%) at follow-up. Clinical features of active disease were absent in 40% of visits at which a new lesion was detected. The mean levels of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) did not differ between the immediate prior visit versus the visit at which a new lesion was detected (ESR mean ± SD= 24.6 ± 4.0 and mean CRP ± SD =12.2 ± 2.8 mg/L at prior visit vs. ESR= 23.5 ± 3.9 and CRP= 9.5 ± 2.8 mg/L at lesion visit, p= 0.63 and 0.12 for ESR and CRP respectively). There were no differences in age, sex, ethnicity, presence of a flare prior to the onset of new lesion, or disease duration in patients with or without new/worse lesions and with or without improved lesions.
Conclusion : Among patients with TAK, large arterial abnormalities are common both at presentation and follow-up. One in 3 patients will continue to develop new or worsening arterial lesions while on treatment with 40% exhibiting no clinical or laboratory changes. Lesions involving the subclavian and carotids are more likely to improve during follow-up. These findings raise concerns about the current definition of active disease in TAK and have implications for the management of patients with TAK and the design and conduct of clinical trials in TAK.
Figure 1. Distribution of arterial lesions at baseline and follow-up visits for patients with Takayasu’s arteritis
To cite this abstract in AMA style:
Sreih AG, Kermani TA, Cuthbertson D, Carette S, Forbess LJ, Khalidi NA, Koening CL, McAlear CA, Monach PA, Moreland LW, Pagnoux C, Seo P, Spiera RF, Warrington KJ, Ytterberg SR, Langford CA, Merkel PA. Longitudinal Angiographic Findings in Patients with Takayasu’s Arteritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/longitudinal-angiographic-findings-in-patients-with-takayasus-arteritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-angiographic-findings-in-patients-with-takayasus-arteritis/