Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) is a severe complication of systemic lupus erythematosus, affecting up to 40% of patients. Unfortunately, about 20% of LN develop end stage renal disease (ESRD) and need replacement therapy. Renal transplantation (RT) may be required. However, concerns about LN recurrence after RT has been reported. In a series of patients with RT due to LN our aim was to assess a) long-term post-transplant survival and, b) comparison of post-transplant survival with a control group due to a non-autoimmune nephropathy, a polycystic kidney disease (PCKD).
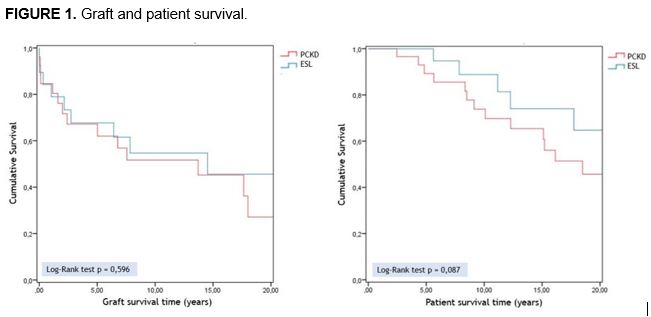
Methods: We studied 2 groups of patients with first RT: a) LN and b) PCKD (control group). All these patients were transplanted in a single reference University Hospital. The main outcome variables were a) graft and patient survival up to 20 years and b) evolution of renal function (serum creatinine and proteinuria) in the first 5 years. Cumulative survival rates after RT were estimated by the Kaplan-Meier method and compared between groups using the log-rank test. Mann-Whitney test or chi2/Fisher’s exact test were used to compare quantitative or qualitative variables, respectively.
Results: We included 53 patients with RT; a) LN group (21), b) PCKD group (32). No significant differences at baseline were observed between both groups regarding sex and cardiovascular risk factors. Significant differences were found in terms of age at RT, with a mean of 39.80±11.27 years in LN group and 46.59±5.01 years in PCKD group (p=0,004). Renal biopsy was performed in 16 LN patients: type II LN (25%), type III (25%) and type IV (50%), according to the World Health Organization and International Society of Nephrology/Renal Pathology Society classification. From 48 patients (of 53) in which a renal biopsy was performed during the first-year post-transplant, rejection was found in 21 cases (43.7%) with no significant differences between both groups (p=0.444). The evolution of serum creatinine and proteinuria after RT is shown in TABLE. Significant differences were found in creatinine levels at the 6th month post-transplant (p=0.032), not so in the rest of measurements. In LN group, 3 patients (14.3%) developed a lupus flare: 2 cases of extrarenal disease and only 1 case with histological recurrence in the graft. No significant differences were found in patient or graft survival between both groups in 20 years of follow-up (Figure 1).
Conclusion: RT may be a safe alternative therapy for ESRD in LN patients and can provide a long-term survival.
TABLE 1. Evolution of creatinine and proteinuria levels after renal transplant.
|
|
1 Month |
6 Months |
1 Year |
3 Years |
5 Years |
|||||
|
Serum Creatinine mg/dL |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
|
N |
28 |
17 |
26 |
15 |
26 |
17 |
22 |
14 |
18 |
13 |
|
Mean |
2.48±2.12 |
1.92±1.41 |
1.82±0.71* |
1.47±0.59* |
1.89±1.03 |
2.03±1.56 |
1.74±1.12 |
2.26±2.51 |
2.06±1.75 |
2.64±3.30 |
|
Proteinuria mg/24 h |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
PCKD |
SLE |
|
N |
24 |
15 |
24 |
12 |
25 |
17 |
21 |
13 |
16 |
11 |
|
Mean |
313.38±218.59 |
581.67±1032.80 |
372.67±375.79 |
651.67±679.01 |
322.84±314.93 |
1426.35±4413.40 |
378.81±383.91 |
409.46±335.64 |
871.81±1498.35 |
487.36±474.62 |
To cite this abstract in AMA style:
Sánchez-Bilbao L, Atienza-Mateo B, Martín-Varillas JL, de Cos-Gómez M, González-Mazón Í, Prieto Peña D, Calderón Goercke M, Ruiz San Millán JC, Rodrigo Calabia E, González-Gay MA, Blanco R. Long-Term Survival of Renal Transplantation Due to Lupus Nephritis. Comparative Study with Non-Autoimmune Transplantation. Study from a Single Center [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/long-term-survival-of-renal-transplantation-due-to-lupus-nephritis-comparative-study-with-non-autoimmune-transplantation-study-from-a-single-center/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-survival-of-renal-transplantation-due-to-lupus-nephritis-comparative-study-with-non-autoimmune-transplantation-study-from-a-single-center/