Session Information
Date: Sunday, November 12, 2023
Title: (0283–0307) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Anti-melanoma differentiation-associated gene 5 (MDA5) antibody-positive dermatomyositis (DM) is frequently complicated by rapidly progressive interstitial lung disease (ILD) and is life-threatening especially in the early stages. Therefore, triple therapy using glucocorticoid (GC), calcineurin inhibitor (CNI) and cyclophosphamide is recently recommended from the early onset. On the other hand, it has also been known that cutaneous symptoms including skin ulcers, papules on the palmar side, and panniculitis are common and afflict patients. However, the long-term prognosis including not only ILD but also the recurrence of skin symptoms is poorly understood. In this study, we assessed the long-term survival rate and recurrence rate in anti-MDA5 antibody-positive DM.
Methods: This retrospective study included patients with anti-MDA5 antibody-positive DM who were admitted to our division from January 2004 to March 2023. Patients who were alive 6 months after the initial hospitalization were classified into the survival group, and those who had died within 6 months were classified into the death group. In addition, the patients were divided into triple therapy (GC, CNI and cyclophosphamide) and GC therapy (GC alone, or GC and CNI). We first analyzed the long-term survival rate in all patients, over 10 years in some patients, and then analyzed it in each group.
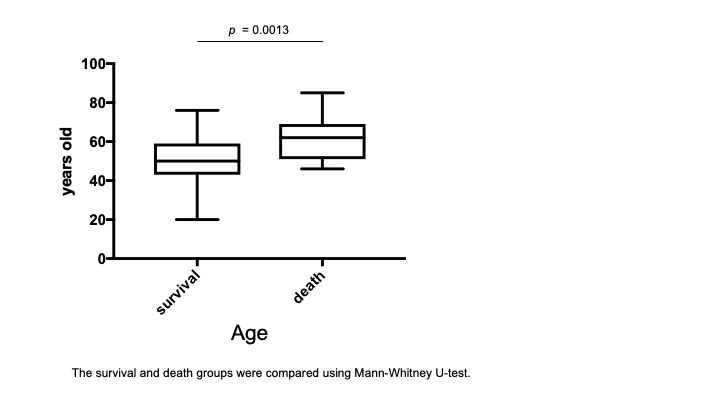
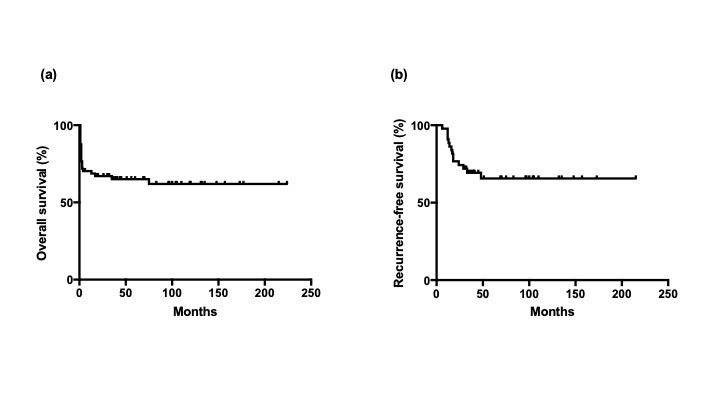
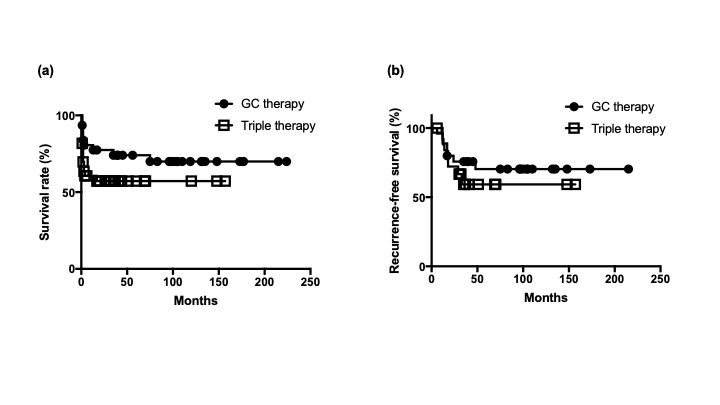
Results: Sixty-eight patients with anti-MDA5 antibody-positive DM were enrolled, two of whom died of malignant tumors within 6 months of onset and were excluded from the analysis. The median age of the patient was 51.5 (range, 20-85 years), and the number of women was 40 (74%). All but one of the 66 patients had ILD. Forty-seven out of 66 patients (71%) were classified into the survival group and 19 (29%) into the death group. The median age of the death group at onset was significantly higher than that of the survival group (62 and 50 years old, respectively, p = 0.0013, Figure. 1). Survival rate declined rapidly to ~70% by 13 weeks after admission but did not decline significantly thereafter (Figure 2 (a)). However, a small number of patients died of ILD one to two years after the onset. Long-term follow-up of the survival group showed that dermatomyositis tended to recur until approximately 50 weeks after the initial admission (Figure 2 (b)). The breakdown of recurrence included not only ILD but also exacerbation of skin symptoms such as skin ulcers. Between triple therapy and GC therapy, there was no significant difference in median age (52.5 and 50 years old, respectively, p = 0.1125), female ratio (55.9% and 65.6%, respectively, p = 0.4182) and serum ferritin levels (658.9 ng/ml and 511.9 ng/ml, respectively, p = 0.2519). Furthermore, there was no significant difference in long-term survival and recurrence-free survival between triple therapy and GC therapy (p = 0.18 and 0.49, respectively, Figure 3).
Conclusion: The survival rate of anti-MDA5 antibody-positive DM rapidly declines by three months after onset. When skin symptoms are also taken into account, the recurrence rate remains relatively high until several years after the onset. There was no superiority of Triple therapy over GC therapy with respect to long-term survival and recurrence rate in this study.
To cite this abstract in AMA style:
Nakamura J, Nagashima T, Sato K. Long-term Prognosis and Recurrence in anti-MDA-5 Antibody-positive Dermatomyositis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/long-term-prognosis-and-recurrence-in-anti-mda-5-antibody-positive-dermatomyositis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-prognosis-and-recurrence-in-anti-mda-5-antibody-positive-dermatomyositis/