Session Information
Date: Sunday, November 10, 2019
Title: Education Poster
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
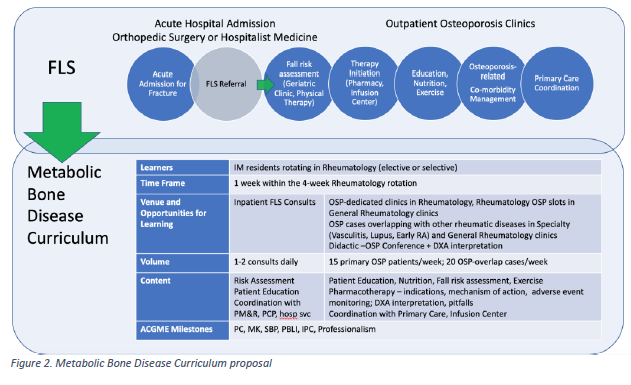
Background/Purpose: Targeting community level health outcomes is one of the higher aims of medical education. Osteoporosis care gaps are prevalent. Only 23% of women with a fragility fracture have dual energy x-ray absorptiometry (DXA) or pharmacotherapy within 6 months post-fracture. There is also an overreliance on DXA for diagnosis, overlooking a history of fractures, underrecognition of osteoporosis in men, and underutilization of fracture risk assessment (FRAX) to guide therapy. A Fracture Liaison Service (FLS) was established after a local institutional study showed similar care gaps. In the context of experiential learning, a metabolic bone disease (MBD) curriculum was designed within the framework of the FLS for Internal Medicine (IM) residents. (Figure 1,2) Areas of emphasis include disease recognition and risk assessment. The objectives of this study are to determine osteoporosis practice care gaps among residents who have undergone the MBD rotation with the goal to inform educators about areas needing curricular improvement.
Methods: IM residents who completed an MBD rotation April 2018-2019 who provided consent for practice habit review were included in the study. Patient encounters from electronic medical records of women > 65 and men > 70 years of age seen for routine followup visits in continuity clinics May 2018-April 2019 were reviewed. Osteoporosis practice guidelines and nationally-defined patient outcome measures were reviewed by faculty. Six parameters on disease recognition (DXA, FRAX or prior fracture), and risk assessment (steroid exposure, vitamin D level determination; also FRAX) were selected by consensus. Descriptive statistics were utilized. The IM Core Program approved the curriculum as a one week block within a Rheumatology rotation in lieu of an independent 4 week rotation.
Results: 52 residents had gone through the rotation during the designated period of time, and 11 agreed to have a practice review. 2, 6, and 3 were PGY 1, 2, and 3, respectively. 88 charts were reviewed of 54 female and 34 male elderly patient encounters occurring within 3 months of MBD rotation completion. (Figure 3) Fifty (57%) DXAs were ordered by 10 residents. 32 DXAs were completed, and 18 (56%) had osteoporosis. Of these 18 cases, prior fracture was documented in 3 (17%) and long-term steroid use in 4 (22%). No chart had documentation of FRAX. Out of 88 charts, 13 (15%) of patients had a vitamin D level checked within 3 months of provider visit or DXA.
Conclusion: Practice review reveals underutilization of osteoporosis diagnosis and risk assessment strategies. Issues to consider for curricular improvement include reformatting the MBD rotation as a 2-week minimum hands-on rotation providing Orthopedic Surgery, Rheumatology and Endocrinology exposure, and increasing active learning components during the rotation and even throughout the year. The FLS aims to engage primary care physicians, and offering learning opportunities for resident continuity clinic supervising primary care faculty also need to be considered.
To cite this abstract in AMA style:
Sandhu, MBBS V, Kamboj A, Duro T, Downey, MD C, Torralba K. Learner Practice Gaps in Osteoporosis: Piloting a Metabolic Bone Disease Curriculum Within a Fracture Liaison Service Framework [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/learner-practice-gaps-in-osteoporosis-piloting-a-metabolic-bone-disease-curriculum-within-a-fracture-liaison-service-framework/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/learner-practice-gaps-in-osteoporosis-piloting-a-metabolic-bone-disease-curriculum-within-a-fracture-liaison-service-framework/