Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Total knee replacement (TKR) is a cost-effective intervention for end-stage knee osteoarthritis (OA). Objectives were to estimate the effect of knee pain severity on willingness to undergo TKR and the impact of healthcare access.
Methods:
The Osteoarthritis Initiative (OAI) is an observational study of participants with or at risk for knee OA. Knee pain severity in the past 30 days was assessed using a numerical rating scale (0-10). Willingness to undergo TKR was ascertained at the 72 month visit. Participants with no history of TKR were included in cross-sectional analyses. Adjusted odds ratios (OR) and 95% confidence intervals (CI) were estimated using logistic regression models. Stratified analyses were conducted to evaluate whether healthcare access modified the association between knee pain severity and willingness to undergo TKR, as well as a likelihood ratio test for interaction between knee pain and components of healthcare access.
Results:
The 3530 participants were predominately White (81.2%) and African American (16.7%), with mean age 66.6 years (sd 9.0), and 58.6% female. More than 90% of participants had health insurance.
Participants with severe knee pain, compared to participants without knee pain, expressed less willingness to undergo TKR (OR 0.70, 95% CI 0.55-0.90) with adjustment for age and sex. This association attenuated after further adjustment for comorbidity, and depression (OR 0.80, 95% CI 0.61-1.03) and when further adjusted for health insurance, prescription coverage, healthcare provider, education, income, employment, race, and marital status (OR 0.92, 95% CI 0.68-1.24).
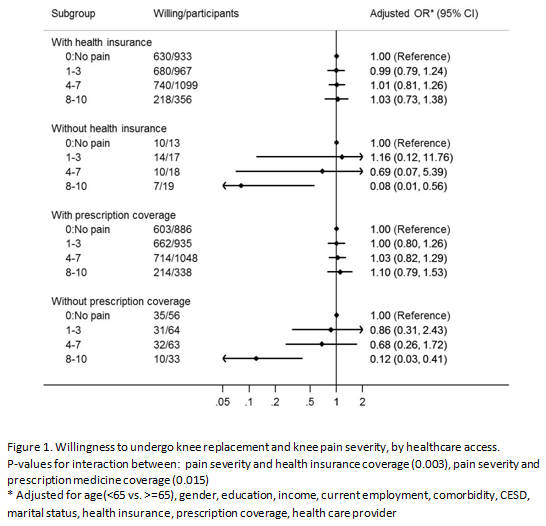
Among participants without health insurance coverage, severe knee pain was associated with significantly decreased odds of willingness to undergo TKR after adjustment for demographic, clinical, healthcare access, and socioeconomic factors (OR 0.08, 95% CI 0.01-0.56) (Figure 1). Similarly, among participants without prescription coverage, those with severe knee pain were significantly less willing to undergo TKR (OR 0.12, 95% CI 0.03-0.41). No association between knee pain and willingness was observed among those with health insurance (OR 1.03, 95% CI 0.73-1.38) and with prescription drug coverage (OR 1.10, 95% CI 0.79-1.53), suggesting that health insurance and prescription drug coverage modify the association between knee pain severity and willingness to undergo TKR (interaction p=0.015 and p=0.003, respectively).
Conclusion:
Among participants with health insurance and with prescription drug coverage, no evidence of an effect of knee pain severity on willingness to undergo TKR was found. Among participants without health insurance and/or without prescription drug coverage, those reporting severe knee pain were less willing to undergo TKR. This finding reinforces the influence of health insurance on preferences and receipt of appropriate medical care.
To cite this abstract in AMA style:
Kaur M, Ashbeck E, Ran D, Kwoh CK, Vina E. Knee Pain and Patient Preference for Knee Replacement: Healthcare Access Matters [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/knee-pain-and-patient-preference-for-knee-replacement-healthcare-access-matters/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/knee-pain-and-patient-preference-for-knee-replacement-healthcare-access-matters/