Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Methods: GENISOS (Genetics versus ENvironment In Scleroderma Outcome Study) cohort patients who had ILD verified by imaging and available pulmonary function tests at enrollment plus 12-18 months thereafter, were included in this study. All patients had disease duration ≤ 5 years at enrollment. FVC, expressed as percentage of predicted value was used as surrogate for severity of ILD. Annualized percent change in FVC at one year follow up was calculated using the formula ((FVC% PFT1 – FVC%PFT0)/FVC%PFT0)/(timePFT1-timePFT0). Baseline demographic, clinical variables and two pneumoproteins, KL-6 and CCL-18 were investigated. KL-6 and CCL-18 were measured by commercially available, validated ELISA kits. Linear regression with baseline clinical and demographic variables as independent variables was performed in univariable and multivariable models.
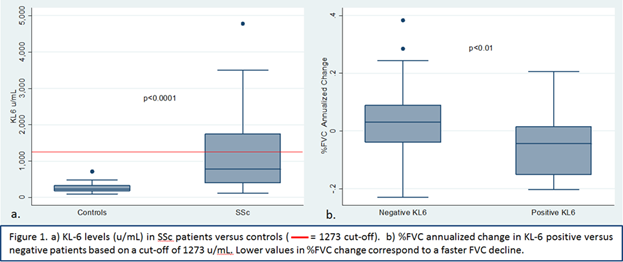
Results: A total of 84 patients with SSc-ILD were included, 19 were male, 19 African-American, and 46 had diffuse disease. Mean disease duration was 2.3 years. Rate of FVC% predicted change over time ranged from -0.23 to 0.38, indicating a highly variable course. Baseline KL-6 levels were higher in patients than in controls (p<0.0001, see Figure 1a). Baseline higher KL-6 levels (as a continuous variable) were predictive of a faster rate of FVC% decline at the one year follow-up (b=-0.03, p=0.04). Upon categorizing KL-6 using a cut-off of 1273 u/mL based on the optimal cut-off previously determined by a Japanese study (Kuwana M et al, J Rheumatol, in press), the predictive significance of KL-6 remained in both the univariate (p=0.01, see Figure 1b) and multivariable analyses after accounting for African-American race, disease duration, age, and treatment with immunosuppressive agents (b=-0.06, p=0.03). Twenty nine (34.5%) patients had KL-6 levels equal or above 1273 u/mL. Although CCL-18 was higher in patients than controls (<0.0001), its levels did not predict rate of FVC decline (p=0.4).
Conclusion: KL-6 but not CCl-18 is predictive of early SSc-ILD progression. In this study, we also validated the proposed cut-off of 1273 for KL-6 in an independent cohort. KL-6 is a promising pneumoprotein that can inform individualized clinical care and contribute to enrichment strategies in clinical trials of SSc-ILD.
To cite this abstract in AMA style:
Salazar G, Kuwana M, Wu M, Ying J, Charles J, Mayes MD, Assassi S. KL-6 and Not CCL-18 Is a Predictor of Early Progression in Systemic Sclerosis Related Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/kl-6-and-not-ccl-18-is-a-predictor-of-early-progression-in-systemic-sclerosis-related-interstitial-lung-disease/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/kl-6-and-not-ccl-18-is-a-predictor-of-early-progression-in-systemic-sclerosis-related-interstitial-lung-disease/