Session Information
Date: Sunday, November 13, 2022
Title: Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Eosinophilic fasciitis (EF) is a rare fibrosing disease. Since described in 1975, less than 30 pediatric cases have been reported. EF presents with painful swelling and progressive skin induration causing peau d’ orange appearance and the groove sign. Laboratory findings include elevated inflammatory markers, aldolase, eosinophils, and immunoglobulin G. EF diagnosis requires biopsy or magnetic resonance imaging (MRI) indicating fasciitis. Risk factors for treatment resistance include concurrent morphea and pediatric age of onset. As triggers, presentation, treatment, and course often differ between pediatric and adult patients, it is important to further characterize juvenile EF cohorts.
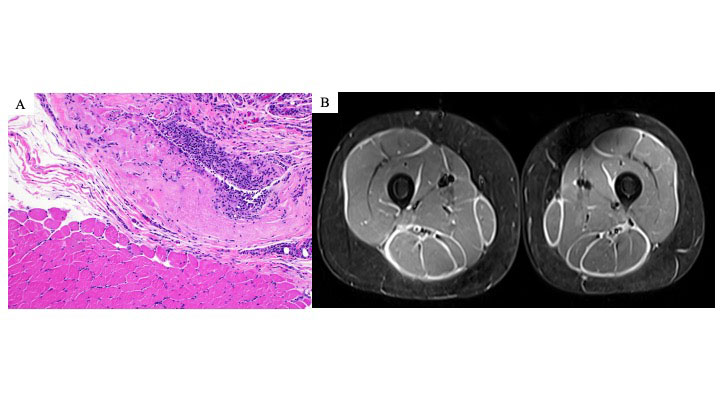
Methods: We report the demographics, clinical findings, pathology, MRIs, treatment, and outcomes for six patients with juvenile EF. A retrospective chart review was performed for all patients diagnosed with EF at our institution between November 2011- May 2022. Inclusion criteria included age at diagnosis < 18 years as well as EF confirmation by histology and MRI (Figure 1).
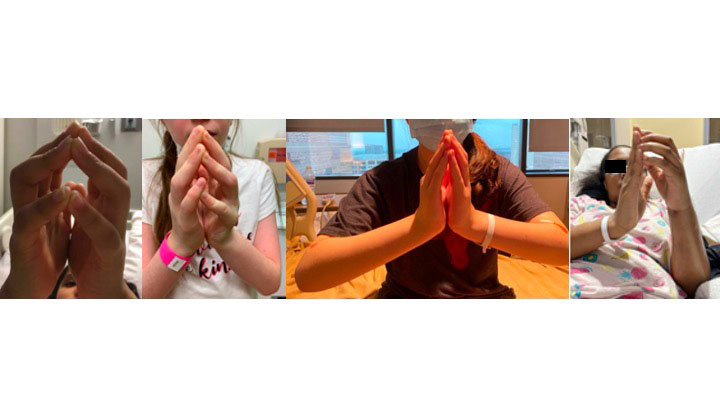
Results: For our juvenile EF cohort, the majority were female (83%) (Table 1). There were 50% Hispanic and 50% non-Hispanic patients. Age at diagnosis ranged from 4-16 years (median: 13) with associated follow-up ranging from 2 months to 12 years. Duration of symptoms prior to diagnosis ranged from 1 month to 1 year (median: 9 months). Associated medical conditions included localized scleroderma (50%), Hashimoto’s thyroiditis, 22q11 deletion, and acquired hemophilia A. Most patients presented with bilateral, progressive painful swelling and severe joint limitation mostly without any positive skin findings; one patient presented with unilateral involvement. All patients presented with a positive prayer sign (Figure 2). Initial treatment included corticosteroids and methotrexate. Other medications included hydroxychloroquine, immunoglobulin, mycophenolate mofetil, rituximab, and tocilizumab. Two patients had relapse of both morphea and fasciitis. Now, 83% are in remission with the remaining patient with resolved musculoskeletal symptoms and an improving factor 8 level after 2 months of treatment.
Conclusion: Juvenile EF can present with swelling and progressive induration without skin abnormalities. Unlike adult cohorts, there were no underlying malignancies or associations with significant trauma. Previous juvenile EF cohorts have described systemic involvement (hepatosplenomegaly, lymphadenopathy), which was not present within this cohort. Although non-specific, the prayer sign could be a helpful clinical finding to identify juvenile EF leading to early recognition and preventing long-term disabling outcomes.
To cite this abstract in AMA style:
Stubbs L, Ogunbona O, Adesina A, Anvari S, Beil E, Lai J, Ramirez A, Szafron V, Ditzler M, DeGuzman M. Juvenile Eosinophilic Fasciitis: A Single-Center Cohort [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/juvenile-eosinophilic-fasciitis-a-single-center-cohort/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/juvenile-eosinophilic-fasciitis-a-single-center-cohort/