Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Isolated axial involvement exists in 2 to 5% of all psoriatic arthritis (PsA) patients. However, it is currently unknown whether patients with isolated axial disease are clinically different than those with concomitant peripheral disease. The primary objective of this study was to determine clinical features associated with isolated axial disease among PsA patients with axial disease irrespective of peripheral involvement. Furthermore, we evaluated predictors for the development of peripheral disease from isolated axial disease over time.
Methods: A longitudinal single center cohort was analyzed to identify PsA patients (all patients fulfilled CASPAR criteria) who had axial disease from January 1978 to October 2020 inclusive, as defined by ≥ grade 2 sacroiliitis bilaterally or ≥ grade 3 sacroiliitis unilaterally on sacroiliac joint radiographs, according to the modified New York criteria. Isolated axial disease was defined by the absence of active/damaged joints or dactylitis. Descriptive statistics determined the percentage of patients with isolated axial and axial with peripheral disease. A logistic regression model determined factors associated with isolated axial disease at initial presentation of axial disease. A cox proportional-hazards model using time-dependent covariates evaluated predictors for the development of peripheral disease from the first presentation of isolated axial disease.
Results: Of the 1576 PsA patients evaluated, 495 (31.4%) had axial disease, of which 32 (2.0%) had isolated axial disease and 463 (29.4%) had concurrent peripheral disease (Table 1). Full protocol information was available for 237 patients for multivariate logistic analysis (Table 2). At initial presentation of axial disease, HLA-B*27 positivity (Odds ratio 25.00, p< 0.003) and lower Health Assessment Questionnaire (HAQ) scores (Odds ratio 0.004, p< 0.010) were associated with isolated axial disease. For the 32 patients with isolated axial disease, univariate cox proportional-hazards model adjusted for sex and age of PsA diagnosis did not reveal any significant predictors for the development of peripheral disease over clinic follow-up (Table 3).
Conclusion: In our PsA cohort, 2.0% patients had isolated axial disease at presentation. At presentation, PsA patients with isolated axial disease had a significantly higher chance of HLA-B*27 positivity. Moreover, those with isolated axial disease compared with concomitant peripheral disease also had lower HAQ scores at presentation, suggesting better functional status. Lastly, there does not appear to be any predictors over time for the development of peripheral disease amongst patients who present with isolated axial disease, though analysis was limited by small sample size.
 Table 1. Clinical Parameters between PsA Patients with Isolated Axial Disease versus those with Concomitant Peripheral Disease at First Presentation of Axial Disease
Table 1. Clinical Parameters between PsA Patients with Isolated Axial Disease versus those with Concomitant Peripheral Disease at First Presentation of Axial Disease
 Table 2. Multivariate Logistic Regression Analysis for Predictors of Isolated Axial Disease at First Presentation of Axial Disease (Nf237)
Table 2. Multivariate Logistic Regression Analysis for Predictors of Isolated Axial Disease at First Presentation of Axial Disease (Nf237)
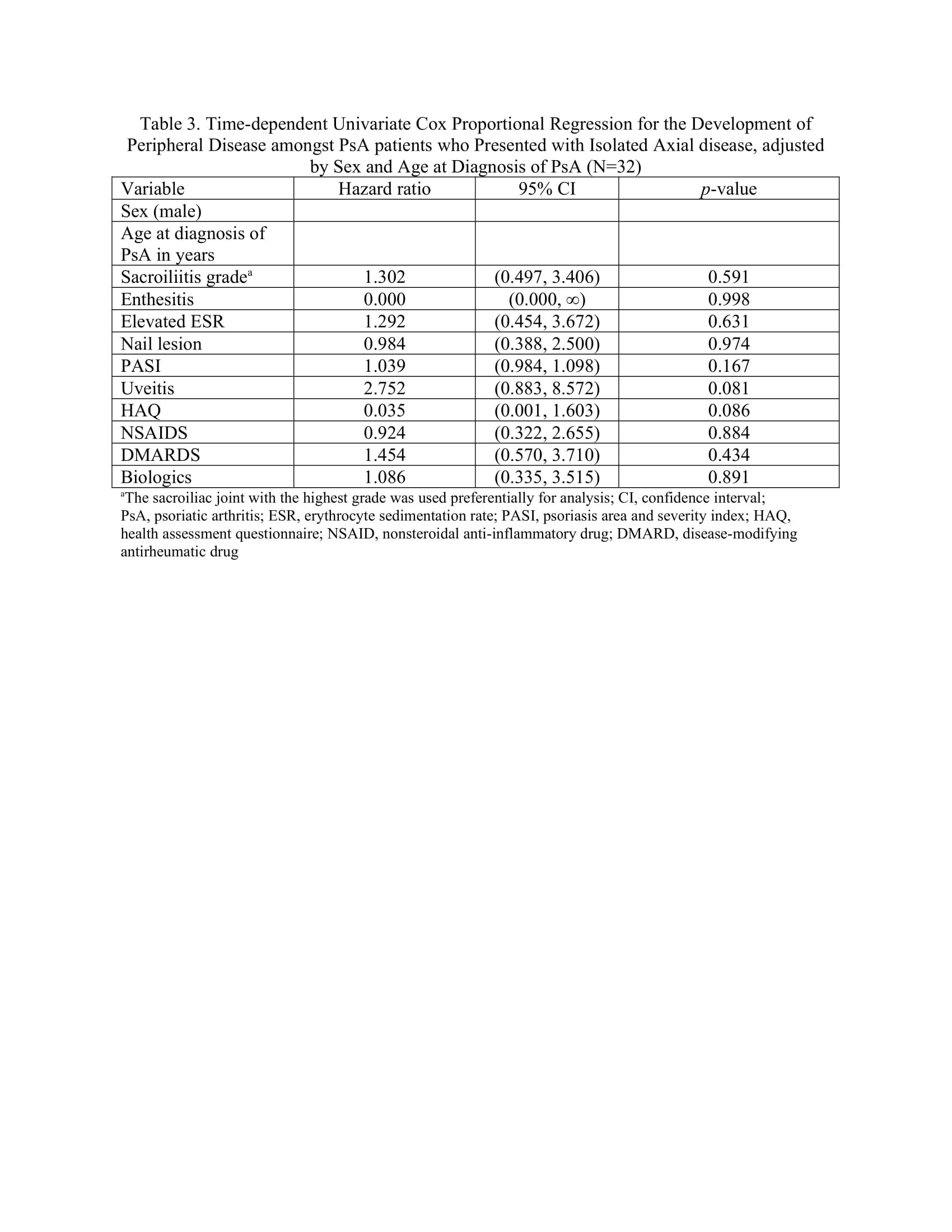 Table 3. Time-dependent Univariate Cox Proportional Regression for the Development of Peripheral Disease amongst PsA patients who Presented with Isolated Axial disease, adjusted by Sex and Age at Diagnosis of PsA (Nf32)
Table 3. Time-dependent Univariate Cox Proportional Regression for the Development of Peripheral Disease amongst PsA patients who Presented with Isolated Axial disease, adjusted by Sex and Age at Diagnosis of PsA (Nf32)
To cite this abstract in AMA style:
Kwok T, Sutton M, Cook R, Pereira D, Gladman D. Isolated Axial versus Concomitant Peripheral Disease in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/isolated-axial-versus-concomitant-peripheral-disease-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/isolated-axial-versus-concomitant-peripheral-disease-in-psoriatic-arthritis/
