Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Systemic vasculitis is a group of uncommon conditions characterized by inflammation of blood vessels, leading to organ ischemia and necrosis. Although several rheumatological disorders such as SLE and Rheumatoid Arthritis are known to increase the risk of myocardial infarction (MI), it is currently unknown if systemic vasculitis is linked to MI. Therefore, we conducted this study to explore the association between Vasculitis and MI.
Methods: To reflect the epidemiology of vasculitis, we included adult patients admitted to teaching hospitals who were more than 40 years of age. For patients with Takayasu Arteritis (TA) and Eosinophilic Granulomatosis with Polyangiitis (EGPA) we included patients above the age of 18. Relevant variables were extracted from the National Inpatient Sample (NIS) using ICD-10 codes from the NIS from 2016 to 2019. We used inverse probability weighting (IPW) with the vasculitis of interest as the treatment and MI as the outcome while adjusting for age, sex, race, family history of MI, Hyperlipidemia, Hypertension, Diabetes Mellitus, Nicotine Use, and Obesity. All the covariates were fully balanced.
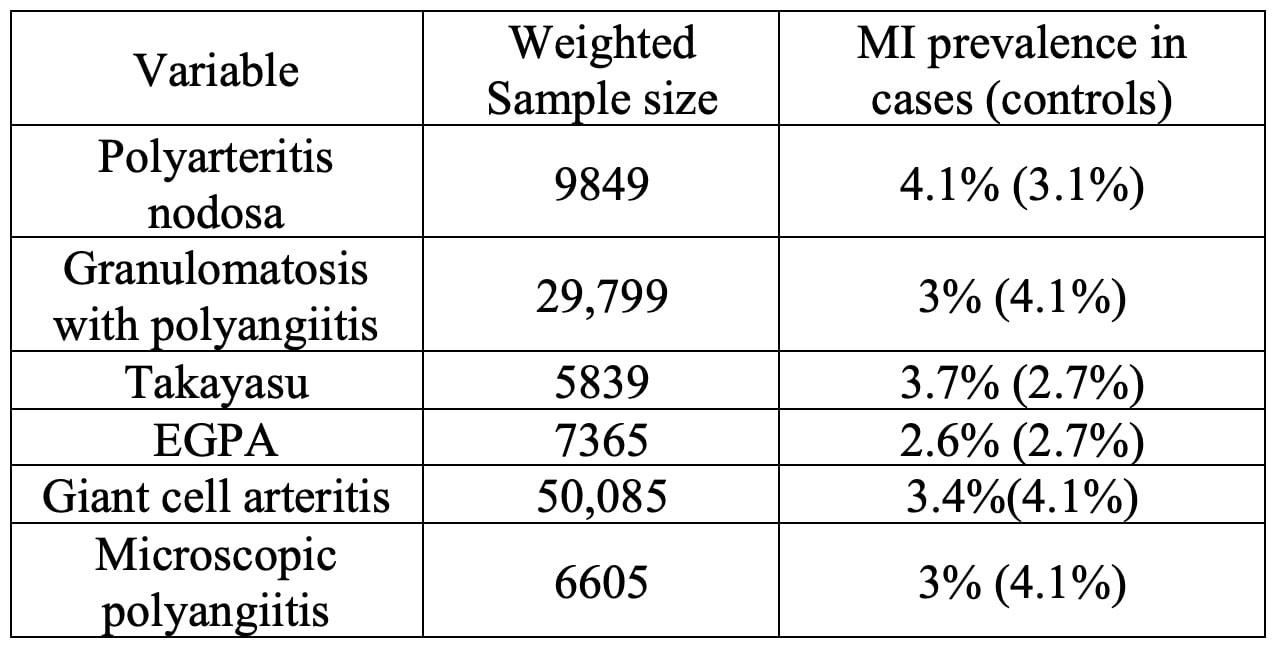
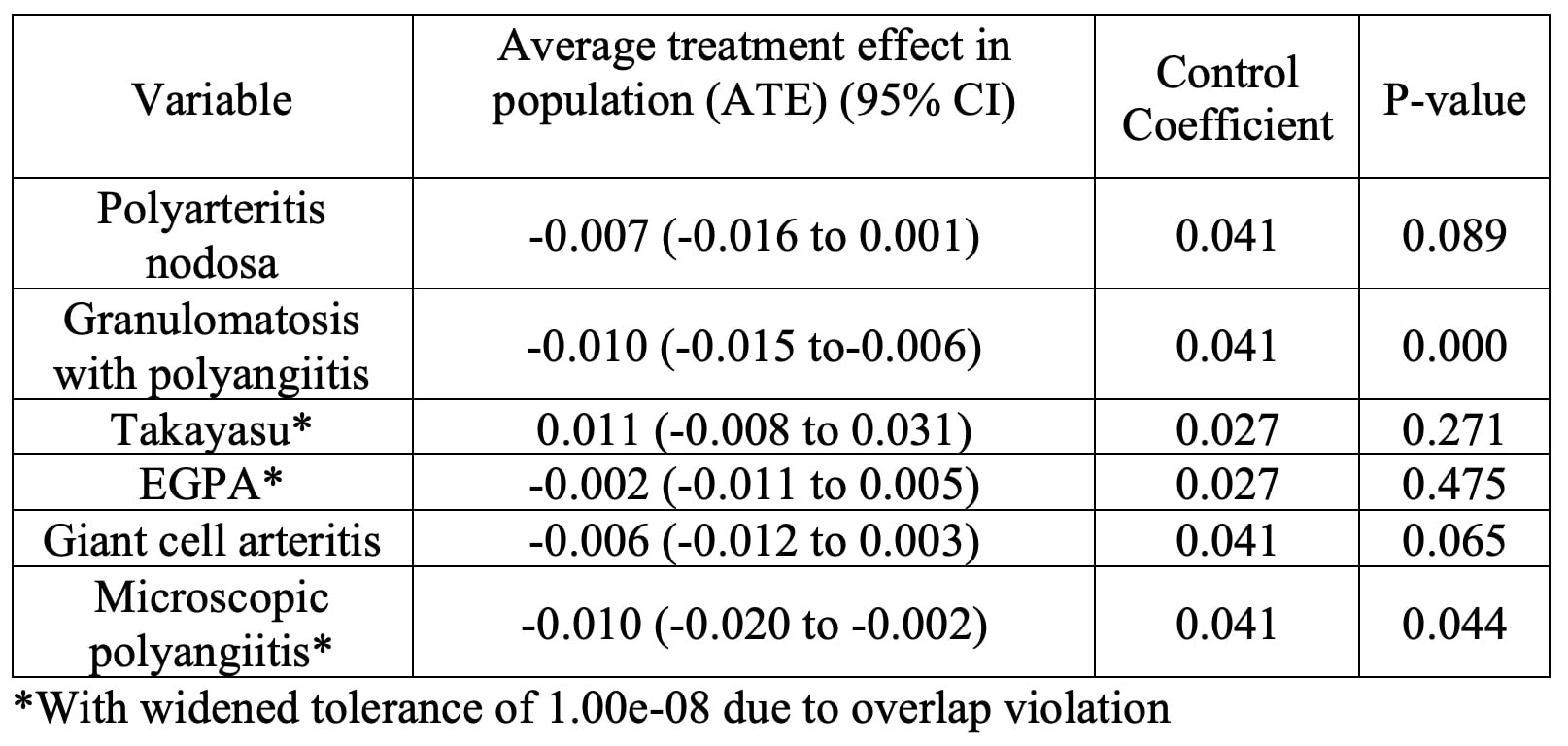
Results: The prevalence of MI was higher in Polyarteritis Nodosa (PAN) and Takayasu Arteritis when compared with controls. The prevalence of MI was lower in EGPA, Giant Cell Arteritis (GCA), Microscopic Polyangiitis (MPA) and GPA when compared with controls. On IPW analysis PAN, Takayasu Arteritis, EGPA, GCA and Microscopic Polyangiitis was not statistically significant for MI (Table 1 and Table 2). GPA and microscopic polyangiitis showed a slightly statistically significant negative association with MI.
Conclusion: The causal link between vasculitis and MI has been proposed by small cohort studies and case reports. One prospective study showed an increased risk of MI with GPA (HR 1.86, 95% CI 1.05-3.31). In another study it was shown that Type 2 MI was more frequently GCA-related than GCA-unrelated (80% vs. 16.7%, p = 0.080), and GCA diagnosis was the only identified triggering factor in 75% of patients with GCA-related Type 2 MI. Some case reports implicate PAN, Takayasu arteritis, MPA and EGPA with MI. However, our extensive study shows that none of the Large-Vessel Vasculitis, ANCA associated Vasculitis and PAN are independently associated with increased risk of MI. The negative association of GPA and microscopic polyangiitis with MI demonstrates only a weak association and has no clinical relevance. Therefore, patients with Large-Vessel Vasculitis, ANCA Associated Vasculitis and PAN should be managed similarly to general population in terms of preventive cardiovascular disease. Key limitations of our study are the retrospective nature, reliance on ICD codes, and the potential for unmeasured confounding.
To cite this abstract in AMA style:
Raj K, Marte Furment M, Verma J, Jyotheeswara Pillai K. Is Systemic Vasculitis a Risk Factor for Myocardial Infarction? A Retrospective Cohort Study from the National Inpatient Sample [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/is-systemic-vasculitis-a-risk-factor-for-myocardial-infarction-a-retrospective-cohort-study-from-the-national-inpatient-sample/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-systemic-vasculitis-a-risk-factor-for-myocardial-infarction-a-retrospective-cohort-study-from-the-national-inpatient-sample/