Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Glucocorticoids are widely used in the treatment of rheumatoid arthritis (RA) patients. It is internationally recommended to taper and stop glucocorticoids as rapidly as clinically feasible, but there are little data regarding this strategy. In two previous clinical trials (BeSt and IMPROVED) patients were treated with methotrexate (MTX) and a temporary course of oral prednisone (60 mg/day, tapered in 7 weeks to 7.5 mg/day). If the treatment target (TT, DAS≤2.4 in BeSt, DAS< 1.6 in IMPROVED) was achieved, prednisone was stopped, but in case of flare it was restarted. We present percentages of successful stopping and looked for potential predictors.
Methods: 508 early RA patients were recruited for the BeSt study, from those 133 patients were randomized into the third arm of treatment (MTX+Sulfasalazin+Prednisone). 610 early RA or undifferentiated arthritis patients were enrolled into the IMPROVED study, all receiving MTX+Prednisone. Disease Activity Score was measured each 3 and 4 months, respectively. Stepwise tapering was slow in BeSt (prednisone tapered only after repeated treatment target achieved, earliest stop at week 35) and more rapid in IMPROVED (prednisone stop as soon as treatment target achieved, earliest at week 16), with a restart in case of flare 3 (BeSt) or 4 months (IMPROVED) after stop, respectively. Percentages still on treatment target after stopping of prednisone were compared in BeSt and IMPROVED. Univariable logistic regression was performed to identify potential predictors of successful stopping. Predictors with p< 0.2 were included in multivariable logistic regression analyses.
Results: In the BeSt study, 67/133 (50%) could stop initial prednisone due to sustained low disease activity (Figure 1). After prednisone stop, 51/67 (76%) patients remained on TT, but 18 flared. In the IMPROVED study, 387/610 (63%) patients stopped prednisone because of DAS-remission at 4 months (Figure 1). Of those, 269/387 (70%) remained on TT after stopping prednisone, while 112 flared. Baseline patient and disease characteristics between patients who did or did not flare after prednisone stop in both studies are shown in Table 1. In the BeSt study, DAS at previous visit was an independent predictor for successful secondary stopping of prednisone (p=0.005, Table 2). In the IMPROVED multivariable testing showed female gender and lower DAS at previous visit as independent predictors of successful secondary stopping prednisone (p< 0.03) Fulfilling the 2010 classification criteria for RA was not associated with the outcome after PRD stop (Table 2).
Conclusion: In these treat-to-target studies, where initial co-treatment with prednisone was stopped after the treatment target was (repeatedly, in BeSt) achieved, a lower DAS at the visit before stopping, was predictive of remaining on treatment target without flare. In IMPROVED, female patients also could more often successfully stop prednisone. Successful stopping of initial co-treatment with prednisone appears to be irrespective of treatment duration and treatment target. The data suggest that in patients with early RA the duration of temporary ‘bridging’ treatment of prednisone should be individually timed.
 Figure 1: flow chart of the patient selection in BeSt and IMPROVED studies. m (month), DF (drug-free).
Figure 1: flow chart of the patient selection in BeSt and IMPROVED studies. m (month), DF (drug-free).
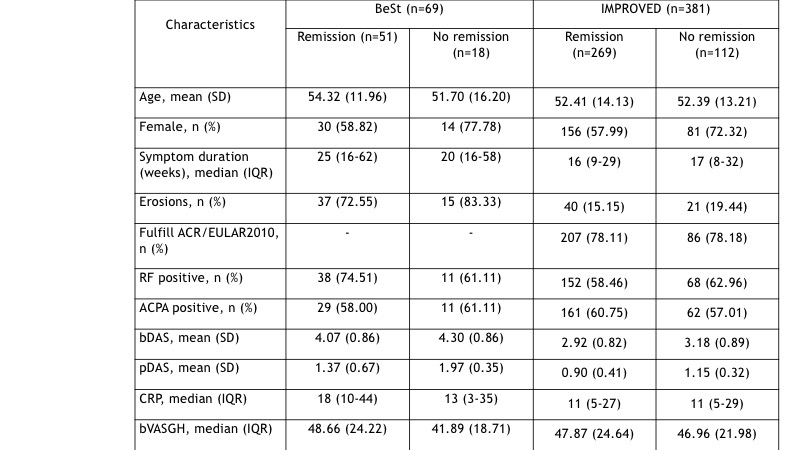 Table 1: baseline characteristics in the BeSt and IMPROVED studies for patients on and off treatment target after stopping prednisone. RF (Rheumatoid Factor), ACPA (Anti-Citrullinated Protein Antibodies), bDAS (baseline DAS), pDAS (previous visit DAS), CRP (C-Reactive Protein, mg/dl), bVASGH (basal Visual Analogue Score Global Health).
Table 1: baseline characteristics in the BeSt and IMPROVED studies for patients on and off treatment target after stopping prednisone. RF (Rheumatoid Factor), ACPA (Anti-Citrullinated Protein Antibodies), bDAS (baseline DAS), pDAS (previous visit DAS), CRP (C-Reactive Protein, mg/dl), bVASGH (basal Visual Analogue Score Global Health).
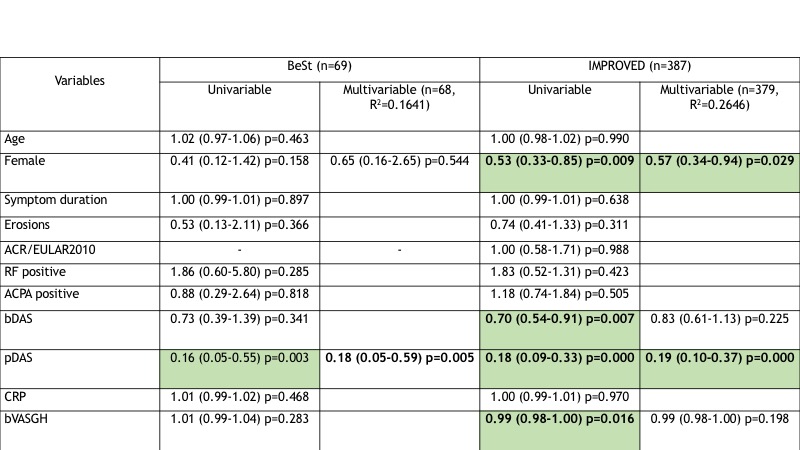 Table 2: univariable and multivariable analysis of predictors for successful GC stopping (OR 95% CI) in the BeSt and IMPROVED studies. RF (Rheumatoid Factor), ACPA (Anti-Citrullinated Protein Antibodies), bDAS (baseline DAS), pDAS (previous visit DAS), CRP (C-Reactive Protein, mg/dl), ∆DAS (difference between DAS at current visit and DAS at baseline), bVASGH (basal Visual Analogue Score Global Health).
Table 2: univariable and multivariable analysis of predictors for successful GC stopping (OR 95% CI) in the BeSt and IMPROVED studies. RF (Rheumatoid Factor), ACPA (Anti-Citrullinated Protein Antibodies), bDAS (baseline DAS), pDAS (previous visit DAS), CRP (C-Reactive Protein, mg/dl), ∆DAS (difference between DAS at current visit and DAS at baseline), bVASGH (basal Visual Analogue Score Global Health).
To cite this abstract in AMA style:
Dos-Santos R, Bergstra S, Maassen J, Huizinga T, Allaart C. Is It Realistic to Stop Prednisone in Early Rheumatoid Arthritis? A Subanalysis from the BeSt and IMPROVED Studies [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/is-it-realistic-to-stop-prednisone-in-early-rheumatoid-arthritis-a-subanalysis-from-the-best-and-improved-studies/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-it-realistic-to-stop-prednisone-in-early-rheumatoid-arthritis-a-subanalysis-from-the-best-and-improved-studies/
