Session Information
Date: Sunday, November 13, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: In radiographic axial spondyloarthritis (r-axSpA), inflammation-driven trabecular bone loss is hypothesised to trigger bone repair at an anatomically distinct site of the same vertebra (the periosteum), i.e., to maintain spinal stability, trabecular bone loss is compensated by syndesmophyte formation. This theory has been difficult to study in patients due to limitations in imaging assessments. Using sensitive imaging techniques such as low dose Computed Tomography (ldCT) and magnetic resonance imaging (MRI), we aimed to investigate whether inflammation is associated with lower bone density (surrogate of bone loss) and subsequently, if lower bone density is associated with a higher likelihood of 2-year bone formation at the same vertebra in r-axSpA.
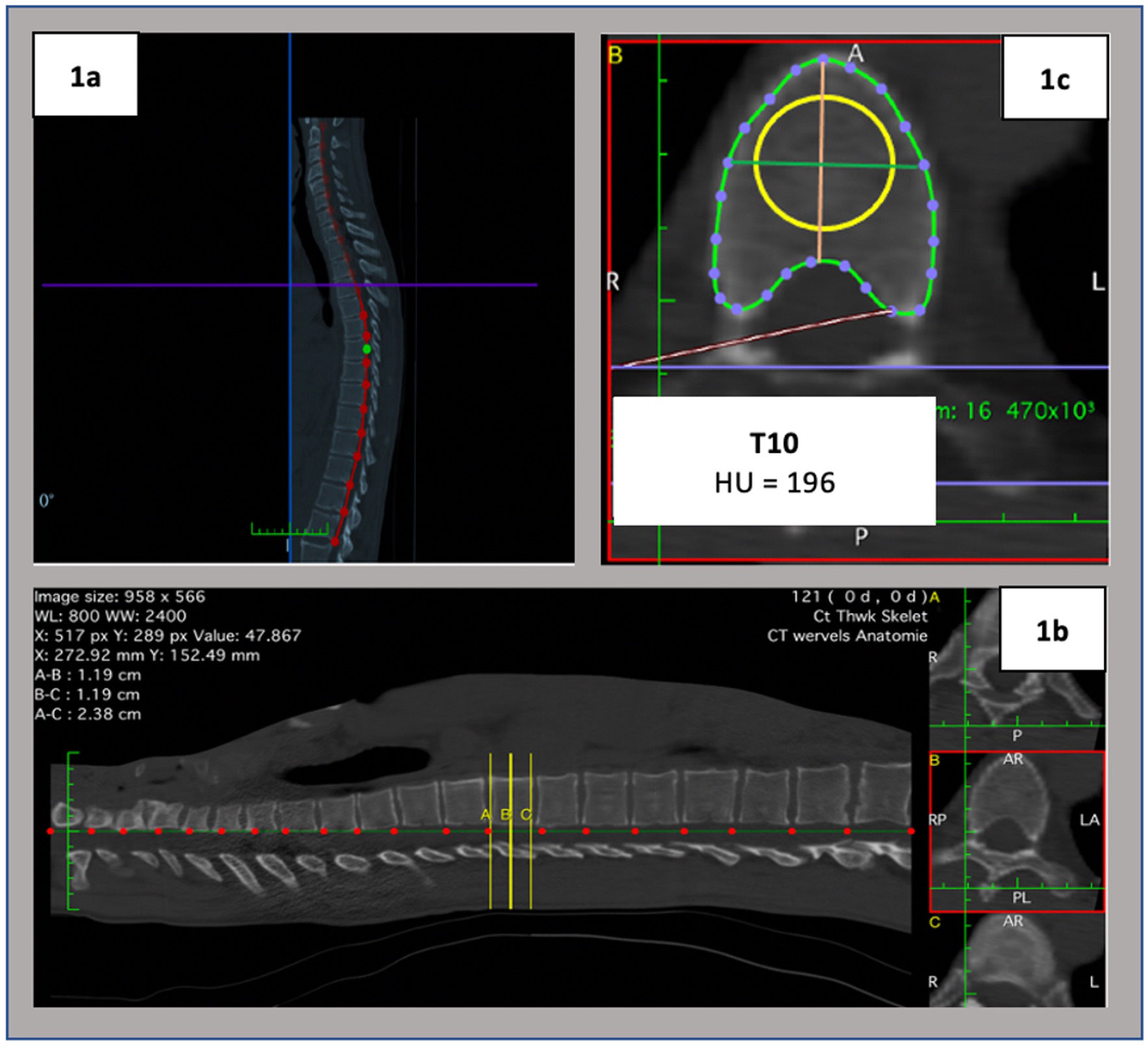
Methods: Data from the multicentre 2-year Sensitive Imaging in Ankylosing Spondylitis (SIAS) cohort was used, including whole spine data from C3 to L5. Baseline vertebral bone density Hounsfield Units (HU) were assessed on ldCT by two readers at each vertebra, using the methodology described in Figure 1. Baseline magnetic resonance imaging bone marrow edema (MRI-BME) status-scores, and 2-year ldCT syndesmophyte formation and/or growth change-scores were assessed by three and two readers respectively. Inter-reader reliability for imaging scorings was assessed by vertebra. Average of readers´ continuous scores or readers´ agreement in binary scores (1-present in ≥1 quadrant/0-absent in all quadrants) were used at the same vertebra. Multilevel generalised estimating equations models were used, the unit of analysis being the vertebra.
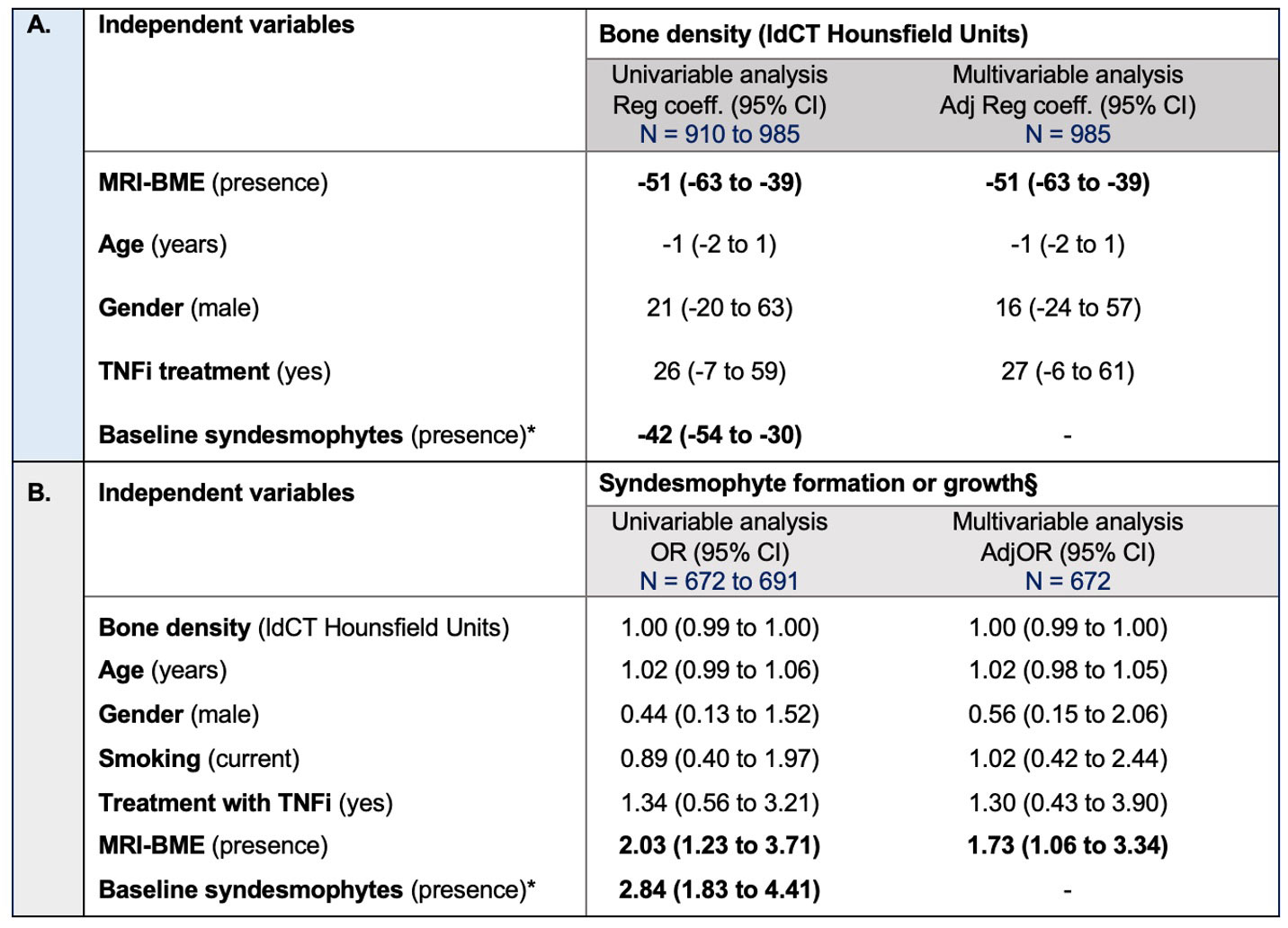
Results: We analysed 1,100 vertebrae in 50 patients with r-axSpA. Intraclass correlation coefficients for HU measurements:0.89-0.97, Fleiss-Kappa (MRI-BME status-scores):0.41-0.78, and Cohen´s kappa (syndesmophyte formation/growth change-scores):0.36-0.74. Bone density HU decreased from cranial to caudal vertebrae. Baseline MRI-BME was present in 300/985 (30%) and syndesmophytes in 588/910 (65%) vertebrae, both most prevalent at the thoracolumbar region. Syndesmophyte formation or growth was observed in 18% of at-risk vertebrae (124/691). A cross-sectional significant confounder-adjusted association was found between inflammation and lower bone density (regression coefficient=-51;95% CI:-63 to -39) (Table 1A). Bone density was not associated with 2-year syndesmophyte formation or growth (adjOR=1.00;95% CI:0.99 to 1.00) (Table 1B).
Conclusion: While in r-axSpA vertebral inflammation is associated with low vertebral bone density, lower vertebral bone density itself did not increase the risk for subsequent bone formation at the same vertebra. These data highlight inflammation as a major factor in r-axSpA bone disease.
SIAS study was funded by the Dutch Rheumatism Association (“ReumaNederland”). MLM is supported by the Fundação para a Ciência e Tecnologia (FCT) grant SFRH/BD/143744/2019.
1a. Sagittal image: selection of spinal curve and vertebral levels identification;
1b. Reconstructed sagittal image: equidistant to A and C, the yellow line B was manually positioned at the center of the vertebral body;
1c. Reconstructed cross-sectional slice at yellow line B level: central circular ROI (diameter=75% of the average of of the average of anteroposterior and transverse diameters) – the density of the vertebra is displayed as the average image intensity within the sample region, reported in HU.
*Multicollinearity with MRI-BME. § Absolute agreement of readers. adjOR, adjusted odds ratio; CI, confidence interval; BME, bone marrow edema, HU, Hounsfield units; ldCT, low dose computed tomography; MRI, magnetic resonance imaging; TNFi, Tumour necrosis factor inhibitors. Statistical significance highlighted in bold.
To cite this abstract in AMA style:
Marques M, Pereira da Silva N, van der Heijde D, Stal R, Baraliakos X, Braun J, Reijnierse M, Bastiaenen C, Ramiro S, van Gaalen f. Is Inflammation-driven Bone Loss Associated with Two-year Bone Formation at the Same Vertebra in Axial Spondyloarthritis? – a Multilevel MRI and Low Dose CT Analysis from the Sensitive Imaging of Axial Spondyloarthritis (SIAS) Cohort [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/is-inflammation-driven-bone-loss-associated-with-two-year-bone-formation-at-the-same-vertebra-in-axial-spondyloarthritis-a-multilevel-mri-and-low-dose-ct-analysis-from-the-sensitive-imaging/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-inflammation-driven-bone-loss-associated-with-two-year-bone-formation-at-the-same-vertebra-in-axial-spondyloarthritis-a-multilevel-mri-and-low-dose-ct-analysis-from-the-sensitive-imaging/