Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Hydroxychloroquine/chloroquine (HCQ/CQ) is considered to be the backbone of systemic lupus erythematosus (SLE) care. Differences in receipt of HCQ/CQ may exacerbate disparities in adverse events, as well as bias observational studies examining the association between HCQ/CQ use and outcomes. We investigated factors associated with first dispensing of HCQ/CQ among individuals with incident SLE. We hypothesized that individuals receiving HCQ/CQ may have better health care access, as measured by outpatient visits and preventive care (e.g., cancer screening and vaccinations), and fewer comorbidities.
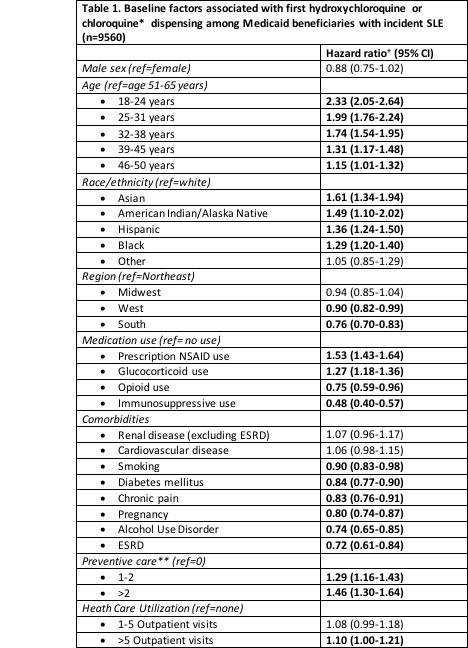
Methods: Using Medicaid claims from 2000-2006 (47 states) and 2007-2010 (29 states), we identified individuals age 18-65 years with incident SLE (>3 SLE ICD-9 codes separated by >30 days within 24 months. We required 24 months of continuous enrollment without SLE codes and without HCQ/CQ use prior to the first SLE code (index date). The primary outcome was the first dispensing of HCQ/CQ on or within 24 months of the index date. We used Cox proportional hazards regression models to examine the association (HR, 95% CI) between baseline sociodemographic factors, comorbidities, health care utilization, preventive care and medication use and time to first HCQ/CQ dispensing in the first 24 months following SLE diagnosis.
Results: We identified 9560 Medicaid beneficiaries with incident SLE; 41% received HCQ (N=3949) or CQ (N=14) within 24 months of diagnosis. The mean age was 35.7 (SD 11.7) years for HCQ/CQ users and 39.9 (SD 12.2) years for non-users. Seventy-two percent received any glucocorticoids within 24 months of diagnosis; of these, 51% also received HCQ/CQ. Cox models demonstrated that younger patients (age 18-25) were 2.3 times more likely to receive HCQ/CQ compared with 51-65 year-olds (Table 1). All racial/ethnic groups were more likely to receive HCQ/CQ than whites. Alcohol use disorder, opioid use, diabetes, end-stage renal disease and smoking were associated with a lower rate of dispensing. Receiving 1-2 preventive care services was associated with 29% higher rate of receipt; >2 with a 46% higher rate. Individuals with more outpatient visits were more likely to receive HCQ/CQ while those with more hospitalizations were less likely.
Conclusion: HCQ/CQ use is central to SLE treatment however only 41% of Medicaid beneficiaries with SLE received HCQ/CQ within 2 years of diagnosis. Preventive care and outpatient visits, markers of access to health care, were associated with higher rates of initial HCQ/CQ dispensing, whereas frequent hospitalizations, high-risk lifestyles and complex comorbidities were associated with lower rates. All non-white races had higher rates of first dispensing compared to whites suggesting that in this Medicaid population, initial HCQ/CQ dispensing differences likely do not explain racial/ethnic disparities in adverse outcomes. Overall these findings suggest that we must cautiously interpret potential physiologic effects of HCQ/CQ on outcomes in observational studies comparing users to non-users as they may be biased by differences in access to care and measured and unmeasured confounders.
To cite this abstract in AMA style:
Pryor K, Xu C, Collins J, Costenbader K, Feldman C. Is Hydroxychloroquine Use a Proxy for Health Care Access? Predictors of First Dispensing Among Medicaid Beneficiaries with Incident Lupus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/is-hydroxychloroquine-use-a-proxy-for-health-care-access-predictors-of-first-dispensing-among-medicaid-beneficiaries-with-incident-lupus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-hydroxychloroquine-use-a-proxy-for-health-care-access-predictors-of-first-dispensing-among-medicaid-beneficiaries-with-incident-lupus/