Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Recent studies have shown that RA patients have increased mortality due to cancer. Despite the increased mortality, few studies have investigated the completion of age-appropriate cancer screening tests in this population. The aim of this study was to determine the cumulative incidence of breast, cervical, prostate, and colorectal cancer screening and evaluate the impact of various demographics and health behaviors on completion.
Methods: We performed a retrospective matched cohort study of patients in southeastern Minnesota with prevalent RA on January 1, 2015. RA patients were identified through review of medical records and fulfillment of either the 1987 ACR or 2010 ACR/EULAR classification criteria. For patients who moved to the region with pre-existing RA, a physician diagnosis of RA with the use of a DMARD was required to be included in the cohort. RA patients were matched 1:1 to randomly selected individuals on sex, age, and county of residence. Age-appropriate cancer screening guidelines for the cancers of interest were determined from the recommendations from the United States Preventative Services Task Force. Cumulative incidence of completion of the recommended cancer screenings was estimated accounting for the competing risk of death, and Cox proportional hazard models adjusted for age and self-identified race assessed for the risk of delay.
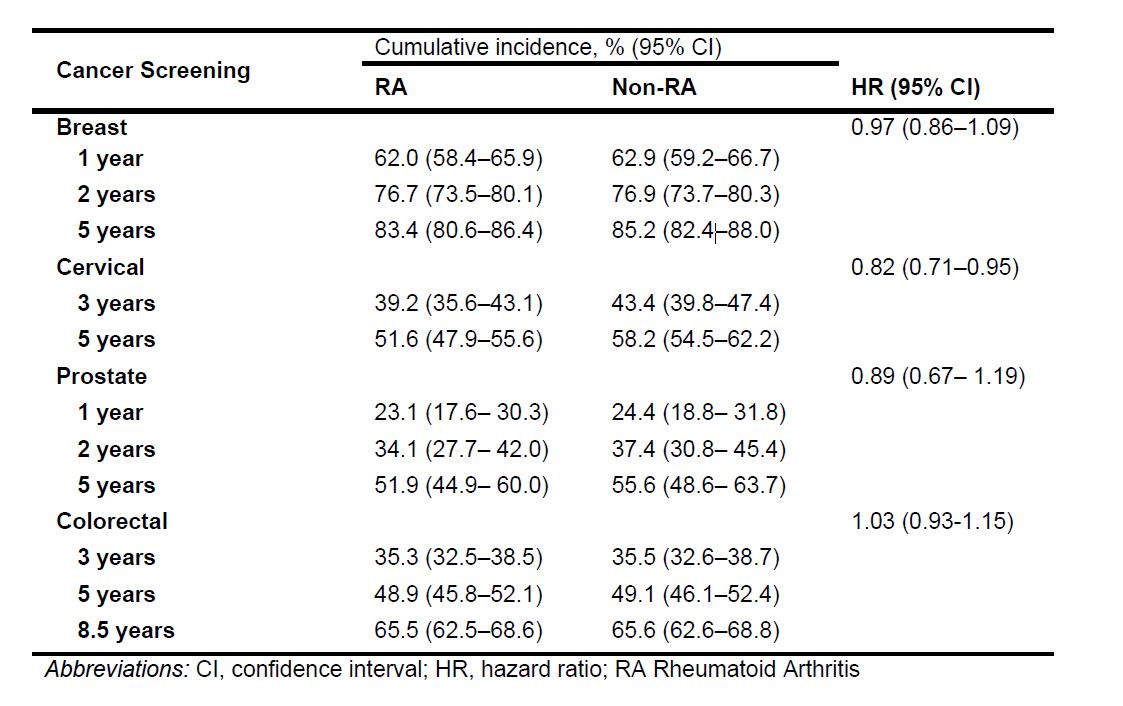
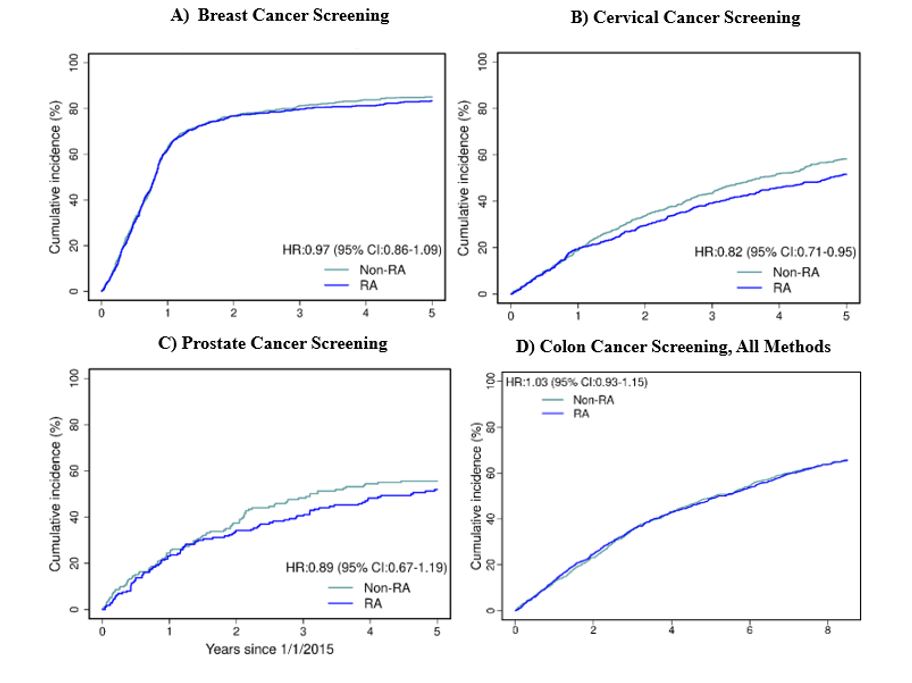
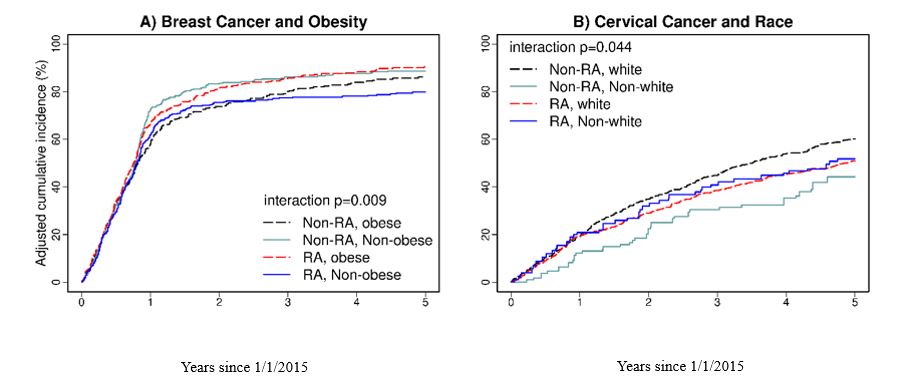
Results: The study included 1,614 patients with RA and 1,597 non-RA comparators, with a mean age of 63 years and 72% being female. After adjusting for age and race, RA was associated with decreased cervical cancer screening (aHR 0.82 [95% CI 0.71-0.95]). However, RA was not significantly associated with a delay in breast, prostate, or colorectal cancer screening (Table 1). At 5 years of follow-up, the non-RA comparators had a higher cumulative incidence of cervical cancer screening compared to RA patients (58.2% [95% CI 54.5-62.2]) vs 51.6% [95% CI 47.9-55.6]) (Table 1, Figure 1). A greater difference in breast cancer screening was observed between obese and non-obese patients with RA compared to those without RA (interaction p=0.009). Interestingly, patients with both RA and obesity had the highest incidence of breast cancer screening. There was a greater difference in cervical cancer screening amongst patients who identified as White and non-White without RA compared to those with RA (interaction p=0.044) (Figure 2). Sensitivity analyses restricted to the years of the COVID-19 pandemic found that the pandemic did not disproportionally affect cancer screening completion amongst those with RA.
Conclusion: RA was associated with an 18% increased risk of delay in cervical cancer screening with the completion in white and non-white RA patients being almost identical. Interestingly, those with both RA and obesity were at a decreased risk of delay in breast cancer screening. These findings suggest that the decreased risk of breast cancer in RA patients could partially be due to increased completion of screening. Importantly, our study suggests that increased attention to cervical cancer screening by both primary care providers and rheumatologists could help to address the excess mortality seen in RA patients due to cancer.
To cite this abstract in AMA style:
Brooks R, Hulshizer C, Hanson A, Kronzer V, Davis J, Myasoedova E, Crowson C. Investigation of Delays in Cancer Screening in RA [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/investigation-of-delays-in-cancer-screening-in-ra/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigation-of-delays-in-cancer-screening-in-ra/