Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with childhood-onset systemic lupus erythematosus (cSLE) have a higher prevalence of depression and anxiety compared to healthy peers. Patients with cSLE also have a 10% greater risk of major depressive disorder (MDD) compared to those with adult-onset SLE (39% vs. 29%). Genetics plays a role in mood disorders and SLE susceptibility. Genome-wide association studies (GWAS) have identified >100 genetic risk variants for depression, as well as for SLE. The cumulative effects of these variants can be combined into polygenic risk scores (PRS). Our study aims to test the association between depression and genetic risk variants for (1) SLE and (2) MDD in a multiethnic cohort of children and adolescents with SLE.
Methods: We included patients followed in the SickKids Lupus clinic from January 1, 2000, to December 31, 2023. All patients met ≥4 American College of Rheumatology (ACR) and/or Systemic Lupus International Collaborative Clinics (SLICC) criteria for SLE with data prospectively collected in a dedicated lupus database. Patients were genotyped on an Illumina multiethnic array, with un-genotyped single nucleotide polymorphisms (SNPs) imputed using TopMed as a referent. Ancestry was genetically inferred using principal components (PCs) and Admixture analyses. We calculated weighted, additive PRSs for: 1) SLE (HLA and non-HLA) and 2) MDD using risk SNPs from the largest GWAS to date. We identified patients with severe depression as those prescribed an antidepressant at any time prior to, or during the course of SLE follow-up. We tested the association between each PRS and depression in univariate and multivariable-adjusted logistic regression models, adjusted for sex and 5 PCs (P< 0.017). We also carried out sensitivity analyses, additionally adjusting for neuropsychiatric lupus (NPSLE) status.
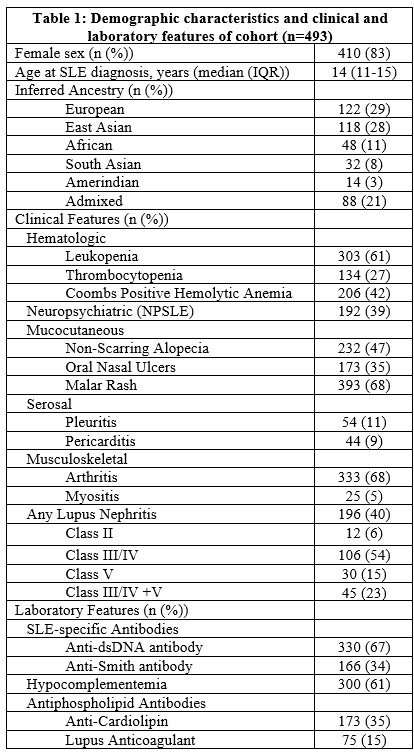
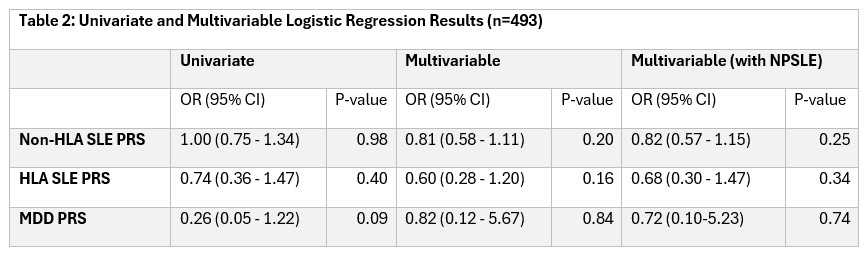
Results: Our study included 493 patients, 83% were female, with a median age of SLE diagnosis of 14 years (IQR 11-15) and 39% had NPSLE. Fifty-one patients were prescribed antidepressants. The majority of patients were of European (29%) and East Asian (28%) ancestry (Table 1). We did not observe a significant association between depression and PRSs for either SLE (HLA and non-HLA) or MDD (Table 2). NPSLE was significantly associated with depression. Sensitivity analyses demonstrated similar associations between PRSs and depression.
Conclusion: In a multiethnic cohort of children and adolescents with SLE, we did not find a significant association between SLE (HLA and non-HLA) and MDD PRSs and severe depression. This may be due to our definition of depression that restricted to patients prescribed antidepressants, which included only 10% of our cohort. Future directions include exploring other case definitions of depression as well as examining anxiety and an additional mood outcome, using validated mood screening tools and clinical chart review.
To cite this abstract in AMA style:
Das I, Gold N, Burton C, Crosbie J, Cao J, Dominguez D, Kronenberg S, Ng L, Toulany A, Tran H, Zai G, Knight A, Hiraki L. Investigating the Genetics of Depression and Anxiety in Children and Adolescents with and Without Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/investigating-the-genetics-of-depression-and-anxiety-in-children-and-adolescents-with-and-without-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigating-the-genetics-of-depression-and-anxiety-in-children-and-adolescents-with-and-without-systemic-lupus-erythematosus/